The Double Empathy Problem In Medicine: Autism, Health, and Communication
By Claire-Eliza Sehinson @nutritionforneurodiversity and Dr. Megan Anna Neff, PsyD (neurodivergentinsights.com)
In a world that values progress in healthcare and inclusivity, the significant health disparities that Autistic people face remind us of the ongoing work needed. To address these disparities and foster a deeper understanding, we, Claire-Eliza Sehinson and Dr. Neff, PsyD—both deeply embedded in the intersection of functional medicine, psychology, and Autistic advocacy—have authored an article to bring to light these critical issues.
To ensure that this information supports Autistic people in their advocacy efforts, we’ve made the guide available for free download. It’s especially designed for Autistic individuals who wish to have more informed and proactive conversations with their healthcare providers. This effort is part of our broader goal to reduce obstacles and contribute to a healthcare environment that is more attuned to and supportive of the specific needs of the Autistic community.
Our article delves into the grave concern of increased early mortality rates among Autistic people, outlines the prevalent obstacles faced in healthcare settings, and presents specific, actionable advice for healthcare providers. It is designed to catalyze meaningful discussions and encourage a shift toward a healthcare system that not only recognizes but actively meets the needs of Autistic individuals.
Our analysis of this problem centers around two critical insights:
The "double empathy problem," which underscores the communication challenges and misunderstandings that often occur between individuals of different neurotypes.
The complex and heightened medical and mental health needs characteristic of Autistic individuals.
These intersecting challenges collide and amplify stress and complicate healthcare experiences for Autistic people. Through this article, we aim to spotlight these issues and suggest practical ways for medical providers to foster a more accommodating and supportive healthcare environment for Autistic individuals.
Early Mortality, Suicidality and Health Disparities in Autistic People
Delving deeper into the health challenges faced by the Autistic community, recent research reveals stark disparities that cannot be overlooked. Early mortality, suicidality, and overall health disparities in Autistic people present urgent concerns as highlighted by the following findings.
A large-scale population based study of over 27,000 Autistic people found life expectancy to be 54 years, compared to 70 years in the general population (a 16 year reduced lifespan). With co-occurring cognitive disabilities this was shortened to 37 years. The three leading causes of death being Suicide, Heart disease and Epilepsy(1).*
Data from UK-based study (2) looking at premature mortality in Autistic people found that that:
Death by suicide was 9 times more likely in Autistic males and 13 times more likely in Autistic females compared to their neurotypical counterparts.
2-fold higher premature deaths from cancer
Where it comes to disease prevalence, Autistic people are
3.3x more likely to suffer from digestive illness
3.5 x more likely to be diagnosed with an endocrine disease and
7.5 x more likely to have a nervous system pathology
Understanding the Impact: A Closer Look at Health Disparities
The statistics highlighted above underscore the grave health inequalities faced by Autistic people in the healthcare system. These disparities not only reflect a significant reduction in life expectancy but also a higher susceptibility to various health conditions compared to the neurotypical population.
It would be easy to overlook these statistics and put them down to stress or just “a part of being Autistic” without further questioning. However, if we examine the rates of heart disease and other conditions that are considered to be related to lifestyle, social and environmental factors rather than purely genetic, and ask why these rates are higher for Autistic people, then it leads to the notion that premature death in Autistic people could actually be preventable.
The research conducted by Dr. Mary Doherty (founder of Autistic Doctors International) and colleagues found that Autistic people face insurmountable barriers when attempting to access appropriate health care. They concluded that because of communication differences, particularly with telecommunications, medical mis-judgements and sensory difficulties in the doctor’s office, physical and mental health conditions can go untreated or present much later in the disease progression leading to more extensive interventions needed (2).
As healthcare providers we know that communication is key in healthcare settings but communication is massively reduced by anxiety, sensory issues and navigating cross neurotype interactions. This means that Autistic people may be experiencing earlier signs and symptoms of cancer, heart disease or mental health difficulties but have an inability to convey distress in a way that is recognizable or believed by medics. This may be leading to delayed diagnoses or opportunity for preventative, life-saving interventions.
Additionally, the sensory difficulties and anxiety generated just from being in healthcare settings means we tend to engage with health professionals only when it becomes life threatening or in the later stages of illness.
The Double Empathy Problem In Medicine
One of the biggest areas of difference in Autistic people is communication. The Double Empathy theory coined by Dr. Damian Milton (an Autistic Sociologist) suggests:
“when people with very different experiences of the world interact with one another, they will struggle to empathise with each other, and this is likely to be exacerbated through differences in language use and comprehension” (3).
Dr. Milton's theory posits that the greater the neurological differences between two individuals, the more challenging it becomes for them to comprehend each other, increasing the likelihood of misunderstandings. This concept emphasizes that communication issues are not one-sided, attributing them solely to the Autistic individual's supposed difficulties in communicating or understanding. Instead, it suggests that miscommunication often arises from a breakdown in cross-neurotype interactions.
The addition of healthcare professionals into the conversation adds another layer to the communication or language “barrier”.** When we train to be doctors, therapists and healthcare providers, we understand the difference between “medical terminology” and layman's terms. We are explicitly taught to communicate medical interventions in layman’s terms to neurotypical patients, but not to neurodivergent people with communication differences.
So there can be an added layer of confusion going both ways. Autistic people may be trying to explain their symptoms in a way that doesn’t match the expectations or textbook training of the healthcare provider.
There are several other ways the double-empathy problem may play out in medical interactions, here are just a few points of considerations:
Communication Challenges
Autistic people’s non-verbal cues might not match our words, leading to misunderstandings. We may not show typical signs of distress like pain or depression.
We may answer health questions very literally, and the broader context of our symptoms may be missed.
Interoception Variability
Differences in sensing internal body states can make it hard for Autistic people to describe pain or discomfort, thus confusing healthcare providers.
Sensory Overwhelm
Overload from bright lights, strong smells, and loud noises in medical settings can make it hard for Autistic people to effectively communicate our concerns.
Co-occurring Conditions
Autistic people often have other conditions that aren't well-understood by doctors, making it harder to get the right care.
Diverse Symptom Presentation
Symptoms may show up differently, risking misdiagnosis or wrong treatment plans because standard symptom guides don't always apply.
Medication Sensitivities
Sensitivities or unusual reactions to medications may not be fully recognized by healthcare providers, affecting treatment choices.
The Triple Empathy Problem
While the double empathy problem highlights significant communication barriers between Autistic people and neurotypical people, the introduction of the triple empathy problem by Sebastian Shaw and team reveals an additional layer of complexity within healthcare interactions. This framework acknowledges that beyond neurology, the intricate nature of medical culture and language intensifies misunderstandings, emphasizing the systemic challenges faced in healthcare settings. This transition signifies a deeper exploration into how these compounded difficulties contribute to the barriers in healthcare access and outcomes for Autistic people.
Struggles Autistic People Can encounter When Engaging Healthcare:
Difficulties grading symptoms on a linear scale from 1-10. For example, pain scales or anxiety scales. I can usually make a case for every number on the scale and it could fluctuate moment to moment.
Telecommunications, especially sitting through long-recorded messages can be stressful. Waiting time can increase anxiety and I am more likely to put the phone down and ignore my symptoms. I cannot always verbalize my needs and can get dismissed.
Neurodivergent people can find it difficult to convey their distress or symptoms verbally. We may have non-sensical descriptions of symptoms like ‘fuzzy’ or ‘vibratey’ which healthcare providers are not able to understand.
We often have impairments in interoception (reduced awareness of bodily sensations until they are urgent or extreme) and may struggle to self-report.
Our non-verbal signs such as facial expressions and body language can be incongruous with the level of distress or pain we are in.
Sensory overload from hospital settings and the doctors office increases anxiety and reduces communication including situational mutism. It can also lead to repercussions to that person’s mental and physical health for days even weeks after the encounter.
Diagnostic overshadowing frequently occurs - whereby the early symptoms of pathology are “over explained” by prior diagnoses - i.e. OCD, anxiety, menopause and not fully investigated.
We have “all-the-things” - Neurodivergent people have higher incidences of a wide range of health vulnerabilities including post-viral fatigue, hypermobility, mental health conditions, mast-cell activation, IBS, allergies, autoimmunity, fertility issues, POTS, chronic pain, PMDD etc. And this complex medical picture can be intimidating for both patient & medical provider.
Understanding Pain in Autistic Individuals: A Complex Communication Challenge
Pain perception and communication about pain can significantly vary among Autistic individuals due to several factors:
Non-Standard Descriptions: Autistic people might not use widely recognized terms to describe pain. Instead, their descriptions could be unique and not easily aligned with conventional diagnostic criteria, making it challenging for healthcare providers to interpret their pain accurately.
Impact of Alexithymia and Flat Affect: Alexithymia, a condition where individuals have difficulty identifying and describing emotions, combined with a tendency towards a flat affect—especially during sensory overload—means non-verbal cues and body language may not reflect the actual intensity of distress. Facial expressions might not show the typical signs of pain seen in neurotypical individuals, leading to a significant underestimation of their discomfort. Additionally, Autistic individuals might exhibit emotional responses that seem out of sync with the context, such as laughing in situations of discomfort, a phenomenon more common among Autistic people.
Interoception Awareness Variability: The awareness of internal bodily sensations, or interoception, can vary greatly. Some Autistic people have low interoception awareness and might not recognize pain until it reaches a high threshold, potentially putting their bodies at greater risk. Conversely, heightened interoception can make the pain experience seem exaggerated relative to the injury, yet the sensory experience of pain is intensely real for the individual.
Understanding these complexities is crucial for healthcare providers. Recognizing the distinct methods by which Autistic people perceive and articulate pain is essential to ensure our healthcare needs are accurately recognized and addressed. It requires the use of non-judgemental curiosity from the provider for the Autistic patient to be believed, understood, and have our needs taken seriously.
Sensory and Emotional Overload
Sensory and emotional overload in healthcare settings contributes to our surmounting anxiety levels and many of us find ourselves situationally mute or lose the capacity to process language or speak coherently. This is not in our conscious control and can impede effective communication in medical visits.
Moreover, the sensory overwhelm associated with medical appointments can significantly distress individuals both before and after the visit. This heightened state of anxiety can disrupt their capacity to attend follow-up appointments or pursue routine care. Such nervous system dysregulation not only affects mental health, leading to fatigue and burnout, but may also trigger shutdown or meltdowns. Consequently, this can further impede the person’s ability to maintain consistent healthcare engagement.
Related Conditions That Impact Our Experience of Health and Communication
Alexithymia and Interoception Differences
Alexithymia and interoceptive differences are both highly prevalent in Autistic people and determine how able a person is to access or verbalise information about their inner state or physical wellbeing.
Alexithymia is a personality trait and an emotional processing difficulty that affects between 40-65% of autistic people (compared to 10% of the general population) and is a byproduct of interoceptive difficulties. In simplistic terms it is the difficulty in expressing or describing emotions or feelings verbally. It is not to be confused with an inability to feel, however some of the difficulties include confusion between bodily sensations and emotions (such as anxiety and urinary urgency) and a tendency towards disconnection from their internal experience (5)(6).
This might manifest clinically as:
The inability to answer feelings-based questions “how does it feel today?” or “on a scale of 1-10 how much discomfort are you in?”
A struggle to describe pain or mental state, sometimes making unusual references or lengthy explanations in an attempt to convey this
They may disclose high emotional reactivity/volatility or only noticing symptoms when they are intense or in severe distress
Poor control of bladder, bowel, impulsivity
Interoception: Interoception is our eighth sensory system and involves the ability to perceive what is happening inside our bodies. We have interoceptive receptors on all major tissues including our heart, stomach, lungs, and skin, which help us sense internal processes such as hunger, thirst, digestion, heart rate, and even the need for deep breathing or relaxation. This internal awareness plays a crucial role in understanding and responding to our body's needs, emotions, and overall well-being.
Interoception plays a significant role in a person’s ability to maintain homeostasis and balance and our fundamental needs (such as oxygen, nutrition or fluid intake). Interoception is gaining recognition for its central involvement in many mental health conditions (including: anxiety and depression, eating disorders, OCD and Substance misuse) as well as physiological illness, including chronic pain conditions i.e. Fibromyalgia, to which there is still no agreed mechanism(4).
Autistic and ADHD individuals are known to have interoceptive and sensory processing differences, which can be high or low. What this means for our health and wellbeing is that if our interoceptive awareness and sensory processing is low, we may not be aware of physiological imbalances or discomfort as quickly as someone unaffected.
Similarly if our interoceptive awareness is very high, this means we can be hypervigilant to sensory input coming from within our own bodies. This can result in our central nervous system interpreting this data as a threat to our safety which generates further physiological consequences via the activation of the stress response, which can also show up as anxiety.
Some clinical examples of how this might show up (not an exhaustive list):
For heightened interoception awareness this may show up as:
Reactivity to multiple foods, medications, environmental factors and supplements that are not immunological
Fibromyalgia
Related to PMDD
IBS all types
Inner tension / high generalised anxiety
Mast Cell Activation Syndrome
Related eating disorders such as ARFID and Anorexia Nervosa
Related to CFS/ME
Related to self-harm and substance misuse
Can manifest as chronic migraines and headaches
For low interoception this may show up as:
Blood glucose instability
Dehydration
Emergency conditions i.e. twisted bowel
IBS-C
Late presentations of stomach ulcers
Poor proprioception and repeated injuries w/ chronic pain (often related to hypermobility and Ehler’s Danlos)
Related to certain eating disorders such as Binge Eating Disorder and Bulimia Nervosa
Related to CFS/ME
Can manifest as chronic migraines and headaches
Unexpected burnout
Missed and mis-diagnosis (diagnostic overshadowing)
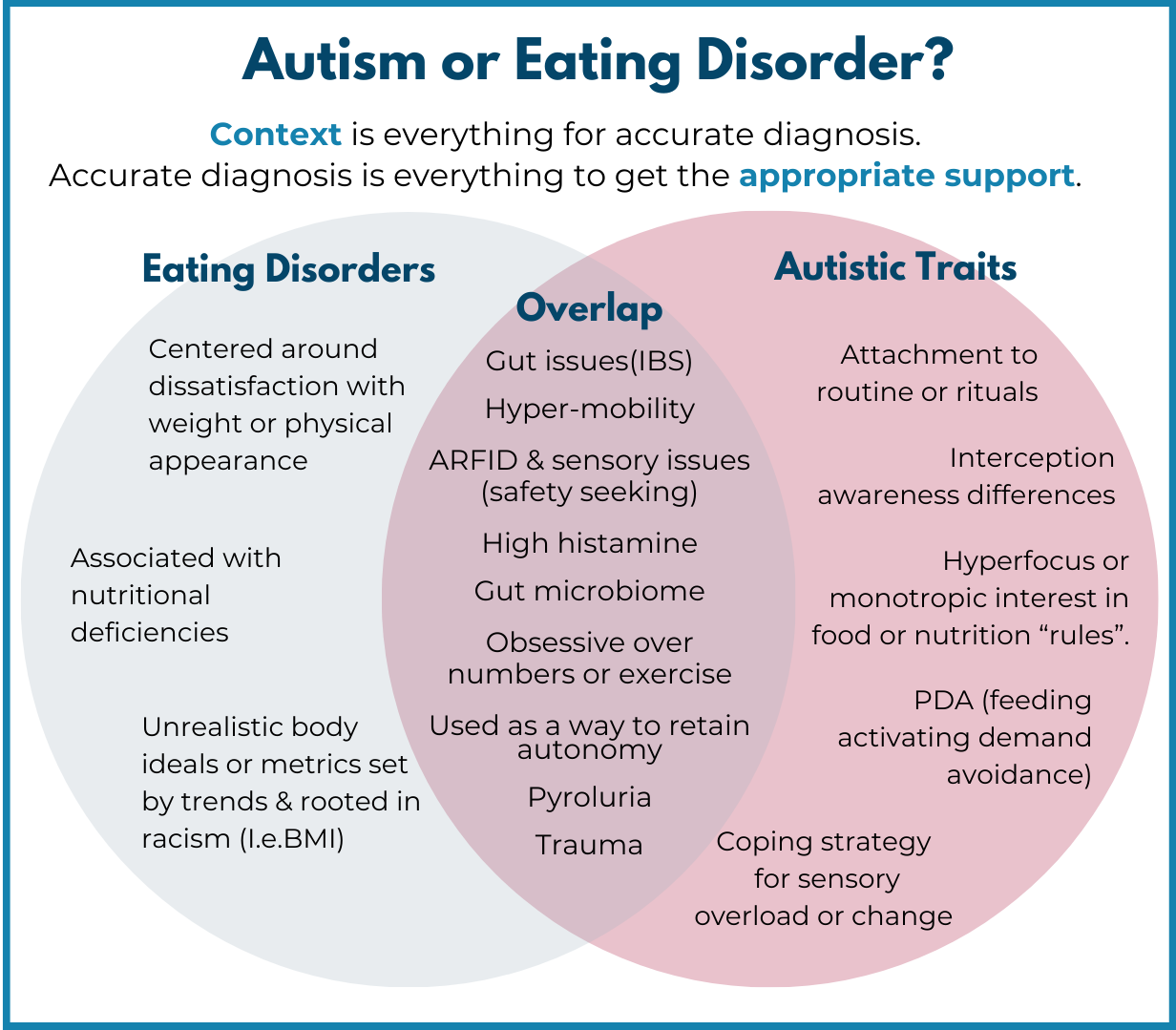
There is significant overlap between the signs and symptoms of many mental health conditions and Autistic traits. For example, the overlap between neurodivergent behaviours, eating disorder criteria and contributing biological factors is significant. So it is not a surprise that figures suggest 20-35% of females with anorexia nervosa may be Autistic(7). We understand that context is needed to obtain an accurate diagnosis in order for evidence-based interventions or treatments to have the best chance to work. Inaccurate diagnoses can lead to more harm.
Understanding why or what function a certain behavior may serve the individual can be the difference between an accurate diagnosis of an eating disorder, or verifying an Autistic trait.
For example, if the attachment to “same foods” and “routine” which give the Autistic person a sense of safety in predictability is misinterpreted for deliberate restriction of food intake to avoid weight gain, then mis-diagnosis can occur. This lack of understanding of context and missed diagnosis of autism can cause further harm to the undiagnosed Autistic person.
Equally, missed-diagnoses can happen in high-masking individuals (especially females and BIPOC) or those who may have a combined neurotype of autism and adhd (AuDHD).
Incidentally, people who are high-masking may present with more interoceptive and trauma responses to stress from social situations or sensory assault from environments such as headaches, gastrointestinal symptoms, allergy symptoms and panic attacks. Masking is understood to be a largely subconscious safety strategy in order to avoid harm. The discomfort of these patients can be labelled as generalized anxiety, other syndromes or “functional disorders” with the possibility of neurodivergence being missed or overlooked.
Pathways Forward: Accomodations and Allyship
Considering the numerous barriers Autistic people face within the healthcare system, we recommend and urge health professionals to introduce introduce a range of accommodations to better support Autistic patients and act as allies. Below is an info graphic providing a list of accommodations for medical providers to consider. Here is a link to the in depth article for further information.
What Can Be Done To Be an Ally?
We highly recommend downloading this very comprehensive report looking at Ways to support effective communication and engagement with Autistic people in healthcare settings.
A summary of recommendations includes:
Always consider the patient could be Autistic and this may not be obvious on first contact. Patients may also be undiagnosed Autistic. A recent study suggested 18.9% of adults in general outpatient mental health clinits met criteria for autism (yet only 0.53% of adults were diagnosed). (8). Consider implementing routine screening into primary care settings.
Adapt the sensory environment to avoid sensory overload.
Adapt communication and avoid bombarding with lots of spoken instructions delivered at a fast pace, allowing additional processing time.
Consider impaired interoception, where Autistic patients might have great difficulty in verbalising or identifying emotions or sensations which can affect what they are able to self-report.
Create predictability and focus where possible. Keeping patients updated with waiting times to reduce anxiety and not-multitasking i.e. speaking and performing a physical exam at the same time.
Be alert to situational mutism - Autistic people, even if hyper-verbal can lose the ability to communicate in the moment.
Have AAC options (alternative augmentative communication) methods available for both non-speaking Autistic people and those with verbal apraxia (inability to execute this skill in the moment).
Consider communication differences as a two-way mismatch (double empathy problem) and put effort to meet them in the middle.
Due to the atypical Autistic facial expressions and body language, always believe what the autistic person is saying about their symptoms and resist making clinical judgements solely based behavioural indicators.
Take a trauma-informed approach - given that Autistic people are more likely to experience trauma than the general population and have often had bad experiences in medical settings.
Offer various methods for accessing services or making appointments given that difficulties with telecommunications is a significant barrier to autistic people accessing help.
Conclusion
The urgent need to address the health disparities affecting the Autistic community cannot be overstated. The significantly reduced life expectancy, heightened risk of suicidality, and increased prevalence of various health conditions among Autistic people underscore a pressing need for a healthcare system that is not only aware of these challenges but is actively working to dismantle them. We hope this article can help Autistic people and medical providers alike understand the various barriers they may experience in navigating healthcare communication and help them to bridge the gap of the double-empathy problem. Through informed advocacy, tailored healthcare strategies, and a commitment to understanding and meeting the complex and heightened medical and mental health needs of Autistic people, we can begin to reduce harm and early mortality.
Footnote:
*The Autistic community, researchers, and clinicians are advised to interpret life expectancy estimates cautiously. This caution stems from the likelihood that undiagnosed Autistic adults, especially those reaching adulthood and older age, might not have been included in the records Baio et al. (2018) used for calculating these estimates.
**Not all medical providers are allistic, in fact some research suggests the medical field is a field that attracts many Autistic people or people on the broader autism phenotype.
References:
Hirvikoski T, Mittendorfer-Rutz E, Boman M, Larsson H, Lichtenstein P, Bölte S. Premature mortality in autism spectrum disorder. Br J Psychiatry. 2016 Mar;208(3):232-8. doi: 10.1192/bjp.bp.114.160192. Epub 2015 Nov 5. PMID: 26541693.
Doherty M, Neilson S, O'Sullivan J, Carravallah L, Johnson M, Cullen W, Shaw SCK. Barriers to healthcare and self-reported adverse outcomes for autistic adults: a cross-sectional study. BMJ Open. 2022 Feb 22;12(2):e056904. doi: 10.1136/bmjopen-2021-056904. PMID: 35193921; PMCID: PMC8883251.
Milton, Damian (2012) On the ontological status of autism: the ‘double empathy problem’. Disability & Society, 27 (6). pp. 883-887. ISSN 0968-7599.
Diest I, von Leupoldt A, Paulus MP; Interoception Summit 2016 participants. Interoception and Mental Health: A Roadmap. Biol Psychiatry Cogn Neurosci Neuroimaging. 2018 Jun;3(6):501-513. doi: 10.1016/j.bpsc.2017.12.004. Epub 2017 Dec 28. PMID: 29884281; PMCID: PMC6054486.
Luminet O, Nielson KA, Ridout N. Having no words for feelings: alexithymia as a fundamental personality dimension at the interface of cognition and emotion. Cogn Emot. 2021 May;35(3):435-448. doi: 10.1080/02699931.2021.1916442. PMID: 33900884
Goerlich KS. The Multifaceted Nature of Alexithymia - A Neuroscientific Perspective. Front Psychol. 2018 Aug 29;9:1614. doi: 10.3389/fpsyg.2018.01614. PMID: 30210420; PMCID: PMC6124373.
Westwood H, Tchanturia K. Autism Spectrum Disorder in Anorexia Nervosa: An Updated Literature Review. Curr Psychiatry Rep. 2017 Jul;19(7):41. doi: 10.1007/s11920-017-0791-9. PMID: 28540593; PMCID: PMC5443871
Nyrenius, J., Eberhard, J., Ghaziuddin, M., Gillberg, C., & Billstedt, E. (2022). Prevalence of autism spectrum disorders in adult outpatient psychiatry. Journal of Autism and Developmental Disorders, 52(9), 3769-3779.
Kassee, C., Babinski, S., Tint, A. et al. Physical health of autistic girls and women: a scoping review. Molecular Autism 11, 84 (2020). https://doi.org/10.1186/s13229-020-00380-z
Shaw, S. C., Carravallah, L., Johnson, M., O’Sullivan, J., Chown, N., Neilson, S., & Doherty, M. (2023). Barriers to healthcare and a ‘triple empathy problem’ may lead to adverse outcomes for autistic adults: A qualitative study. Autism, 0(0). https://doi.org/10.1177/13623613231205629
Baio, J., Wiggins, L., Christensen, D.L., Maenner, M.J., Daniels, J., Warren, Z., Dowling, N.F., ... (2018). Prevalence of autism spectrum disorder among children aged 8 years - Autism and developmental disabilities monitoring network, 11 Sites, United States, 2014. MMWR Surveillance Summaries, 67(6), 1-23.