Autism and Health Issues Unpacked: Exploring the Intersection of Autism and Chronic Fatigue Syndrome
Autism Overview
Do you ever find yourself navigating the maze of persistent fatigue, mysterious GI issues, hormonal sensitivities, and sensory sensitivities, wondering if these are linked to autism, chronic fatigue, or something else? You’re not alone. You’re not alone. Many in the Autistic community, including Autistic physician Mel Houser, refer to these myriad health complexities accompanying an Autism diagnosis as “all the things.”
In this article, we, two Autistic professionals—a psychologist and a functional medicine provider—aim to unravel the intricate connections between Autism and Chronic Fatigue Syndrome/Myalgic Encephalomyelitis and other health conditions. We bring our clinical expertise and personal experiences to this complex intersection, hoping to clarify and illuminate the parallels and unique challenges faced by individuals dealing with both conditions.
From the prevalence of chronic fatigue and burnout in the Autistic and ADHD communities to the interconnected co-occurrence in CFS/ME, we explore the shared vulnerabilities and the risk of diagnostic overshadowing. Ultimately, we seek to differentiate between autism and CFS/ME, understand their overlaps, and underscore the need for accurate support and interventions.
This content, resembling an encyclopedia entry, delves into a wide range of health-related topics, rich in complexities and nuances. Feel free to dive into specific sections that pique your interest or browse through for a general understanding of various themes. This approach allows you to tailor your reading experience to your needs, whether you’re seeking detailed information or an overarching summary.
It’s a lot of information, so feel free to skim ahead to the relevant sections.
Jump to ....
Autism: A Distinct Neurotype
Autism is a distinct neurotype, characterized by a distinct and sensitive nervous system. This distinctiveness can sometimes lead to confusion with nervous system disorders like CFS/ME, complex trauma, and other dysautonomias.
Characteristics of Autistic Individuals
Autistic people have a specific way of perceiving and interacting with the world. This includes direct communication, a highly sensitive nervous system, a tendency for monotropic attention, self-soothing through repetition and routine, and a communication style marked by authenticity, directness, and literal language use.
The following are several experiences and conditions that often occur within the constellation of autism:
PMDD
Executive Functioning Differences
Genetic Conditions
Autistic Burnout
ARFID and Eating Disorder
Significant sensory processing diferences
Alexithymia and interoception challenges
PMDD (Premenstrual Dysphoric Disorder)
PMDD is a severe form of premenstrual syndrome characterized by significant mood swings and physical symptoms. This condition is often due to a genetic cellular sensitivity to changes in estrogen and progesterone levels. Studies indicate varying prevalence rates of PMDD among Autistic AFAB individuals, ranging from 14.5% to 92%. This significant variance underscores the impact PMDD has on mental health in this population, including a heightened prevalence of suicidal thoughts and attempts (Citation: Groenman, 2022)).
Executive Functioning Differences
Executive functioning encompasses a group of cognitive skills crucial for planning, organizing, initiating tasks, managing time, and regulating behavior. Many Autistic people experience differences in these areas, significantly affecting our daily life. These differences are particularly challenging when navigating health contexts, managing medications, and maintaining medical regimens. Understanding these challenges is vital in grasping how autism impacts an individual’s experience of other health conditions.
It’s important to note that while individuals with CFS/ME may also face executive functioning challenges, these are typically due to the illness itself and not a baseline characteristic. In contrast, Autistic individuals often have inherent difficulties with executive functioning. These challenges may intensify during periods of Autistic burnout or when dealing with co-occurring conditions, but they are a fundamental part of their baseline experience.
Genetic Conditions
In addition to their neurotype, some Autistic individuals may have co-occurring genetic conditions, including Prader-Willi syndrome. This rare genetic disorder affects growth, metabolism, and behavior. Although Prader-Willi syndrome’s prevalence is low in the general population, a significant overlap exists with autism. Research indicates that 12-26% of individuals with Prader-Willi syndrome also exhibit autistic traits (Bennett, 2015; Kong et al., 2020).
While most Autistic individuals do not have Prader-Willi syndrome or other specific genetic conditions, the occurrence of these conditions is higher among Autistic people compared to the non-autistic (allistic) population. Current recommendations suggest that genetic testing for conditions like Prader-Willi syndrome can be beneficial following an autism diagnosis in childhood, due to the higher rates of co-occurrence.
Autistic Burnout
Characterized by exhaustion from masking autistic traits and coping with daily demands, autistic burnout can significantly affect mental health and resembles the fatigue seen in chronic fatigue syndrome.
ARFID or History of "Eating Disorder"
ARFID, or Avoidant/Restrictive Food Intake Disorder, is characterized by a limited range of food choices stemming from:
Avoidance of specific sensory characteristics in food, such as textures or smells.
Aversions to certain foods or the feeding environment, often as a trauma response to prior experiences like choking, force-feeding, or pain.
Restrictions due to low appetite, disinterest, or a lack of enjoyment in food.
Many Autistic individuals across all age groups may experience ARFID or have a history of eating challenges. These challenges are often misinterpreted as other eating disorders, like Anorexia Nervosa, or simply dismissed as “picky eating.” These feeding issues can contribute to or be caused by gastrointestinal (GI) problems, interoceptive difficulties, and can exacerbate nutritional deficiencies or other health conditions (Schmidt et al, 2021).
Although current research suggests a prevalence rate of ARFID in Autistic individuals at around 16%, this figure is likely a conservative estimate. Clinical experience indicates that this number is probably much higher. ARFID has only been formally recognized since the publication of DSM-5 in 2013 and is still predominantly considered a pediatric condition. However, a broader understanding acknowledges that ARFID affects individuals of all ages. For many undiagnosed Autistic individuals, feeding behaviors may represent their initial interaction with the medical system. Further exploration of these issues will be discussed in our upcoming blog post on Gut Health, ARFID, and sensory eating.
Alexithymia
Alexithymia, characterized by difficulties in recognizing and expressing emotions, is notably more prevalent in the Autistic community. Estimates suggest that approximately 50% of Autistic individuals experience alexithymia. This condition is not only about emotional recognition and expression but also has broader implications for overall health. Alexithymia is associated with an increased incidence of chronic pain, burnout, somatization, and other chronic health conditions (Aron, 2019; Kojima, 2012).
Significant Sensory Issues/SPDs (Sensory Processing Differences)
Sensory processing differences are indeed a defining characteristic of autism. Many Autistic individuals experience either heightened or diminished sensitivities to various sensory inputs, such as light, sound, touch, or taste. Additionally, differences in interoception, the internal perception of bodily sensations, are common, with some experiencing reduced awareness or an amplification of internal signals.
These sensory processing differences play a crucial role in shaping the daily experiences of Autistic people, profoundly impacting their interaction with health and illness. Such sensitivities can extend to gastrointestinal discomforts, influencing eating habits and potentially leading to issues like ARFID. Moreover, heightened or altered sensory perceptions can also affect hydration, as the sensory qualities of liquids might be challenging for some. These nuances in sensory processing are not just isolated experiences; they directly contribute to the overall management and navigation of various health conditions, underscoring the need for tailored approaches in healthcare and daily living strategies.
While it’s true that sensory processing sensitivities can develop in anyone undergoing chronic illness, for Autistic individuals, these sensitivities are typically present from childhood. They constitute a core part of their baseline experience. Notably, these sensitivities may intensify during periods of Autistic burnout or when facing additional health challenges.
Language and Auditory Processing Differences
Autistic people often exhibit distinct language and auditory processing differences. These differences can result in challenges with typical (allistic) communication styles. Autistic brains generally process information in a bottom-up, detail-oriented manner. This means that Autistic individuals might process their environments and information more deeply, and sometimes more slowly, compared to non-autistic individuals.
This bottom-up processing style and distinct approach to language and communication are key factors that distinguish autism from CFS/ME and other conditions primarily affecting the nervous system. The unique nature of Autistic communication has been observed in the way Autistic people often relate more naturally with each other. This distinctive communication style and mutual understanding amongst Autistic individuals can be considered a cultural difference, reflecting a shared experience and perspective within the Autistic community (Crompton et al., 2020).
Distinct Autistic Brain Style
Similarly, the Autistic brain style is distinctly its own, characterized by a distinct way of processing information and perceiving the world. This distinctive approach influences various aspects of life for Autistic individuals, from how they engage in social interactions to their methods of problem-solving, to self-soothing through routine and repetition. This is also a distinguishing feature from other nervous-system based conditions such as Chronic Fatigue Syndrome.
Present from Birth
Finally, a critical distinguishing factor of autism lies in its etiology. Autism is a neurotype that is inherently present from birth, deeply embedded in an individual’s neurological framework. This innate aspect sets it apart from conditions like CFS/ME, which typically develop later in life. Understanding autism as an intrinsic part of an individual’s neurology from the outset is essential, as it underscores the fundamental differences between autism and other conditions that emerge over time.
Chronic Fatigue Syndrome Overview
Chronic Fatigue Syndrome (CFS), also known as Myalgic Encephalomyelitis (M.E.), is a chronic, multifactorial neurological disease characterized by a spectrum of symptoms impacting various body systems.
Key Diagnostic Characteristics of Chronic Fatigue Syndrome
Debilitating Fatigue: A profound level of fatigue that is not relieved by rest and severely impacts daily functioning.
Cognitive Difficulties: Often referred to as “brain fog,” this encompasses challenges with memory, concentration, and overall cognitive processing.
Sleep Disturbance: Difficulties in both falling asleep and maintaining restful sleep.
Post-Exertional Malaise: A significant worsening of symptoms following physical or mental exertion.
It’s important to keep in mind that the experience of ME/CFS varies among individuals. Not everyone will have the same set of symptoms or follow the same progression of the illness. Furthermore, there are additional symptoms that often present with ME/CFS.
Additional Recognized Symptoms
The complexity of ME/CFS is further evident in a range of associated symptoms, including but not limited to:
Chronic pain
Orthostatic Intolerance or POTS (Postural Orthostatic Tachycardia Syndrome)
Autonomic Dysfunction
Temperature Sensitivity
Neuromuscular Symptoms (such as twitching and myoclonic jerks)
Flu-like Symptoms and recurrent viral infections
Intolerance to alcohol or certain foods
Heightened sensory sensitivities
Gastrointestinal difficulties
These symptoms are officially recognized in the NICE (National Institute for Health and Care Excellence) guidelines, highlighting the multifaceted nature of ME/CFS and its profound impact on those affected.

Variability and Impact
ME/CFS is marked by its variability in severity and daily fluctuation of symptoms, significantly disrupting all aspects of life, including social interactions, work, and personal relationships. The condition’s unpredictability and profound psychological impact make it particularly challenging. A 2008 study by Dancey highlighted that individuals with CFS experience greater disruption to their lives than those with other chronic and severe illnesses, including anxiety disorders, cancer, and multiple sclerosis (M.S.).
Current Understanding and Treatment Approaches
To date, there is no consensus on the underlying disease mechanism of ME/CFS, nor is there a cure. Treatment focuses primarily on managing symptoms. However, ongoing research is shedding light on possible contributing factors, including immune and autonomic nervous system dysfunction, neuro-endocrine disorders, gut microbiome imbalances, genetic predispositions, and metabolic abnormalities, such as mitochondrial dysfunction.
Diagnosis: Adult or Rapid Onset (Not Present Since Birth)
ME/CFS is often underdiagnosed, with an estimated 80% of cases going unrecognized. On average, it takes about five years from the onset of symptoms for a patient to receive a diagnosis. Contributing to this challenge is the variability in clinical definitions and criteria for diagnosing ME/CFS.
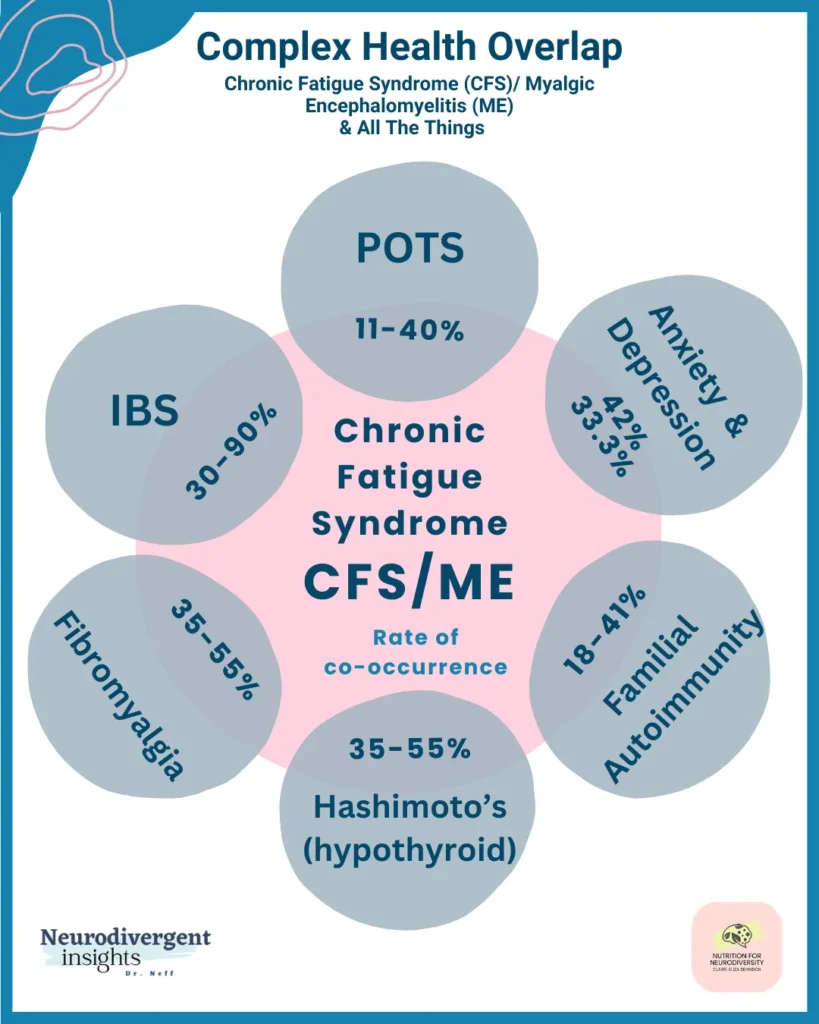
Common Comorbid Health Conditions
In addition to its primary symptoms, up to 97% of individuals with ME/CFS also contend with one or more comorbid health conditions, which may include:
POTS (Postural Orthostatic Tachycardia Syndrome)
Anxiety and Depression
IBS (Irritable Bowel Syndrome)
Fibromyalgia
Hashimoto’s Thyroiditis
Various Autoimmune Disorders
Reference: Afari et al., 2003; Castro-Marrero et al., 2017; Chu et al., 2019; Daniels et al., 2017 Chu et al., 2019; Daniels et al., 2017
Chronic Fatigue Triggers
One notable distinction between ME/CFS and autism is its development later in life. While genetic predispositions can increase susceptibility to ME/CFS, the condition is often precipitated by specific events. These triggers, if not properly addressed, can perpetuate and exacerbate symptoms throughout the illness. Key triggers include:
Viral or Bacterial Infection: Researchers like Hickie et al. (2006) have found that infections can initiate ME/CFS, suggesting a link between the immune response and the onset of symptoms.
Autoimmunity: According to Sotzny (2018), autoimmunity plays a role in ME/CFS, indicating that the body’s immune response against its own tissues may contribute to the condition.
Mycotoxin and Mold Illness: Brewer et al. (2013) highlight the impact of environmental factors, specifically mycotoxins and mold, in triggering ME/CFS, showing the condition’s sensitivity to external biological agents.
Genetic Variants in Biological Pathways: Wang et al. (2017) point to specific genetic variations that affect immune and neurotransmitter systems, which can predispose individuals to ME/CFS.
Stress and Occupational Burnout: Recent findings by Springer et al. (2023) demonstrate a correlation between prolonged stress, occupational burnout, and the development of ME/CFS, underscoring the interplay between psychological stressors and physical health.
Emotional Trauma: Emotional trauma is also recognized as a potential trigger, reflecting the complex interaction between mental health and physical well-being in ME/CFS.
Correlated with High Adverse Childhood Events (ACES) and PTSD
Psychological factors are integral in the complex web of health challenges associated with ME/CFS. Notably, experiences of childhood trauma, including sexual, physical, and emotional abuse or neglect, as well as conditions like depression and anxiety, significantly increase the risk of developing CFS in later life. This risk is magnified in the presence of PTSD symptoms, as detailed in studies like Heim (2009), which report a six-fold increase in risk.
The persistent stimulation of the biological stress response, specifically the HPA axis (hypothalamic pituitary axis), due to developmental trauma or PTSD, leads to altered sensitivity. This change means the stress response doesn’t “switch off” as easily, resulting in symptoms like hyper-vigilance and hyper-reactivity to minor or non-existent threats, or what can be described as a “loss of resilience”.
Correlation with Personality Traits
Further, studies exploring personality traits in ME/CFS have shed light on increased risks associated with certain characteristics. For instance, Buckley (1999) found that individuals with ME/CFS were often more “hard driving”. Lievesley et al. (2014) reported higher personal and parental expectations during childhood among this group. Additionally, Magnusson et al. (1996) linked the negative aspects of perfectionism in individuals with ME/CFS to maladaptive coping strategies.
This evidence underscores the profound impact of psychological experiences and traits on the development of ME/CFS, suggesting that both childhood experiences and personality factors can significantly influence the risk and experience of the condition.
Occupational Triggers And Risk Factors
Clinical observations suggest that certain professions may be more susceptible to developing ME/CFS. This heightened risk is often linked to exposure to environmental toxins, chemicals, or infections, especially in specific geographical areas. These occupational hazards can interact with genetic predispositions, which might be previously undetected, and are often exacerbated by lifestyle factors like inadequate sleep and high stress levels.
Military Service and Gulf War Syndrome
Military personnel exemplify this risk. Soldiers frequently face sleep deprivation, intense physical training, and considerable psychological stress, all while being exposed to diverse microbial, chemical, and biological threats.
A notable instance is Gulf War Syndrome (GWS), often called “the ME of the military.” GWS, affecting about 50% of Gulf War veterans, shares over 30 symptoms with ME/CFS. Although its cause remains medically unexplained, studies such as Chao et al. (2014) have linked it to brain volume shrinkage associated with low-level organophosphate exposure, affecting regions related to emotions, the autonomic nervous system, and sensory processing.
Industrial Work and Heavy Metal Exposure
The industrial sector poses similar risks. Exposure to heavy metals like cadmium, a common environmental and occupational pollutant, has been linked to neurological symptoms similar to those of ME/CFS. Research, including Pacini et al. (2012), indicates that cadmium exposure can adversely affect memory, attention, and energy levels. The highest cadmium exposure risk is seen among industrial workers, residents of heavily industrialized areas, and cigarette smokers.
Recognizing the connection between certain occupations and ME/CFS risk is crucial for preventive measures and providing targeted support and treatment for those impacted by such occupational hazards.
Autism and Chronic Fatigue Syndrome: Overlapping Experiences
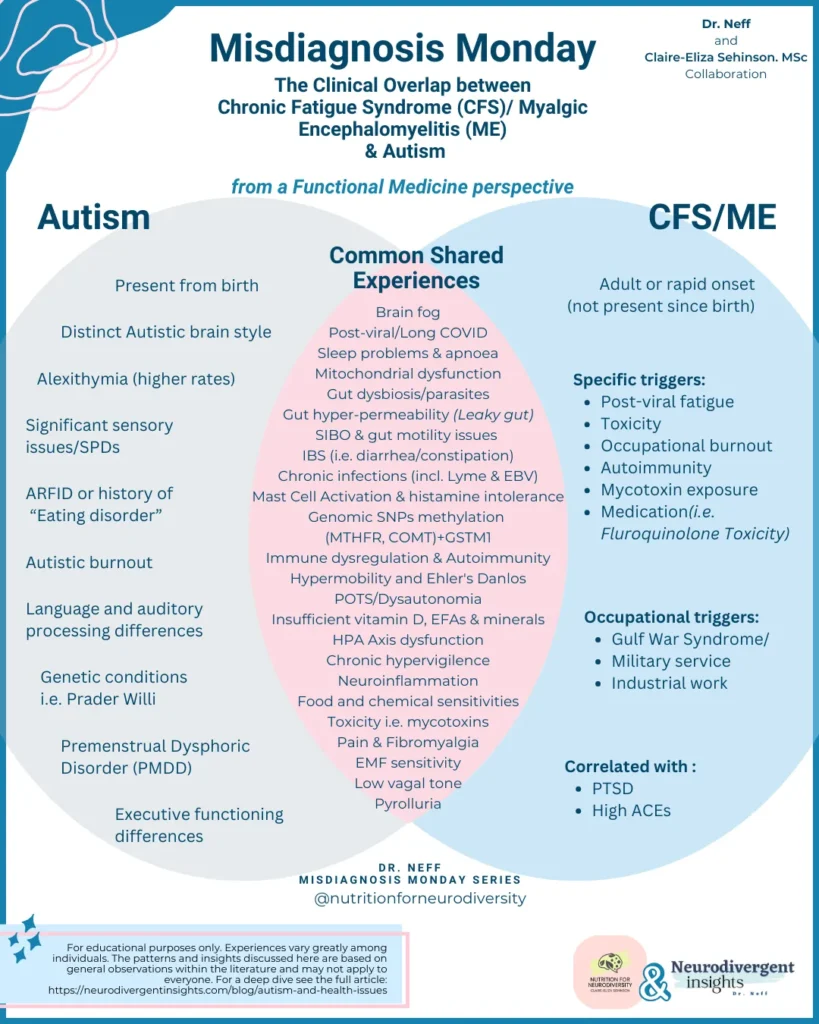
As highlighted by the Venn diagram, there are significant overlaps between autism and Chronic Fatigue Syndrome (CFS/ME), often leading to diagnostic overshadowing. Let’s explore some of these shared experiences:
Brain Fog
Brain fog is a widely used term encompassing various symptoms of cognitive and executive dysfunction, commonly seen in ME/CFS and other chronic illnesses. Typically, it includes:
Confusion
Mental fatigue
Lack of clarity
Disorganization
Concentration difficulties
Slowed information processing
Newly apparent memory issues
In Autistic people, many symptoms associated with brain fog often surface during periods of sensory overload, stress, shutdowns, and meltdowns. Hormonal fluctuations, such as those occurring during cyclical changes or transitions like perimenopause/menopause, can also exacerbate these symptoms. Moreover, brain fog is a recognized feature of conditions like anxiety and depression, with potential links to infection and neuroinflammation.
Brain fog is not exclusive to autism or ME/CFS; it’s also a common element in other health conditions, including long COVID. Importantly, brain fog should not be an experience people are expected to “just live with.” Appropriate accommodations and healthcare support, targeting the underlying causes, can significantly alleviate these symptoms.
Post-Viral/Long COVID and Its Connection to ME/CFS
The historical link between ME/CFS and infectious diseases has been well-documented. Notable examples include the “cluster outbreaks” of ME/CFS, such as the Royal Free Hospital Outbreak in London in 1955 and the Nevada (Incline Village) outbreak in 1985 (Acheson,1959).
Research indicates that a variety of microbial infections can lead to a chronic fatigue symptom profile persisting long after the acute infection phase (Hickie et al., 2006). Interestingly, up to 12% of people may experience prolonged illness post-infection, a statistic mirrored in Long-COVID prevalence data from the UK, where approximately 1 in 10 COVID-19 cases result in persistent illness (Atchinson et al., 2023).
Long-COVID and post-viral ME/CFS share nearly identical clinical characteristics, with emerging research suggesting Long-COVID may be an immune subtype of ME/CFS. This is supported by overlapping pathological processes observed in both conditions.
Furthermore, individuals in the neurodivergent community, both diagnosed and undiagnosed, have been reported to face a higher risk of Long-COVID or COVID-related health complications (All Brain’s Belong).
Immune Dysregulation & Autoimmunity in Autism and CFS/ME
A key factor in the post-viral fatigue and complications observed in both Autistic and CFS/ME patients is “immune dysregulation” and autoimmunity. Similar Immune Abnormalities in CFS/ME and Autism including:
Insufficient Antiviral Defense: One notable similarity is the reduced number of Natural Killer (NK) Cells in both autistic and CFS/ME patients. NK cells, a type of T-lymphocyte, are crucial for eliminating viral infections and monitoring early cancer processes. Effective infection control is closely linked to the count and function of these cells (Espinosa et al., 2019)(Sarasella et al., 2023)
Autoimmunity Trends: Another observation is the higher incidence of autoimmune conditions within families of both Autistic and CFS/ME individuals, hinting at a genetic predisposition (Sotzny, 2018). Autoimmunity is a complex disease process where the immune system, which typically balances defense and tolerance, becomes dysfunctional. This breakdown in immune communication leads to the mistaken attack and destruction of healthy tissues. Numerous lifestyle factors can influence the progression of autoimmune diseases – these include vitamin D levels, nutrition, sleep quality, and stress. We plan to explore these modifiable factors in future articles.
Chronic Infections and Their Impact on Autism and CFS/ME
The Role of Stealth Infections
Both Autistic and CFS/ME individuals commonly encounter chronic and persistent infections. Notably, the herpes virus family, including Epstein-Barr Virus (EBV), Cytomegalovirus, HHV-6, Herpes Simplex, along with hepatitis and enteroviruses, play a significant role in the ongoing disease process in ME/CFS. These viruses often target either neurons (“neurotropic”) or immune cells (“immunotropic”), leading to the neurological and immune-related symptoms frequently observed. Their ability to evade immune detection makes them particularly challenging to address (Rasa et al, 2018).
Chronic Infections in Autism Research
Research has shown a significant correlation between chronic infections and Autistic individuals. However, there is a notable challenge in this area of scientific study. Often, the narrative mistakenly frames autism as a disease. This perspective can divert attention away from a crucial understanding: chronic infections in Autistic people may often be a consequence of underlying immune dysfunction and decreased resistance, which are more common in this population. Importantly, this understanding steers us away from the misleading notion that chronic infections in childhood are a cause of autism. Recognizing and maintaining this distinction is vital for practicing medicine and health therapies within a neurodivergent-affirming paradigm.
Opportunistic Infections and EBV
While 95% of the general population may have been exposed to EBV, most are asymptomatic. However, individuals with chronic fatigue are more susceptible to illnesses from such opportunistic viruses due to underlying immune dysfunction and decreased resistance.
The Interplay of Stress and Viruses
Cortisol, the stress hormone, has been shown to reactivate EBV and other herpes viruses (Yang et al., 2010). Consequently, post-viral fatigue may follow periods of high stress, burnout, or constant sensory overload, which is particularly relevant for Autistic individuals facing daily sensory challenges.
Infections and Behavior
While PANS/PANDAS is a complex topic beyond the scope of this article, it’s worth noting that this area is highly relevant to Autistic health, especially in children, and deserves attention in discussions about autism and health.
Understanding Sleep Issues in Autism and ME/CFS
Sleep difficulties and unrefreshing sleep are a near constant feature of autism and affect between 85-90% of people with ME/CFS where sleep issues can precede the onset of illness by years.(Gotts et al., 2013). This research outlines many types of sleep disorder patterns that can occur, including:
Sleep Disorders in Autism and ME/CFS
Prevalence: Between 85-90% of people with ME/CFS face sleep difficulties. Similarly, 50-80% of Autistic children experience sleep disorders, significantly higher than the 9-50% in neurotypical children (Reynolds et al., 2019; Gotts et al., 2013).
Circadian Rhythm Disorders: Many Autistic individuals have mutations affecting their circadian rhythms, yet autism is often overlooked in CRSWD (Circadian Rhythm Sleep-Wake Disorders) diagnoses.
Melatonin Regulation in Autism: A common feature in autism is a mutation in melatonin-regulating genes, leading to altered sleep cues at night and increased sleepiness during other parts of the day (Furfaro, 2020).
Obstructive Sleep Apnea and Periodic Limb Movement: Around 30% of individuals with ME/CFS meet criteria for conditions like obstructive sleep apnea or periodic limb movement. These conditions are also more common among Autistic people.
Insomnia or Hypersomnolence: Significant rates of insomnia or excessive sleepiness are reported in both ME/CFS (89.1%) and autism (Furfaro, 2020).
Impact of Disrupted Sleep Stages:
Within these groups different stages of sleep i.e. REM sleep or stage 3 may be disrupted. For example, Autistic individuals on average spend about 15% of their sleep in the REM phase, compared to 25% in neurotypicals. REM sleep, crucial for learning and memory, is therefore often reduced in autism (Buckley et al., 2010; Neumeyer et al., 2019). In autism, poor sleep can intensify repetitive behaviors and hyperactivity, creating a cycle where these behaviors further disrupt sleep.
Each sleep phase serves critical health functions, and disruptions in these stages can impair different biological processes. The architecture of normal sleep is influenced by several factors, including daylight exposure, dietary habits, physical activity, insulin secretion, ambient temperature, and hormonal levels, particularly melatonin and cortisol.
The box below outlines physiological factors that can contribute to sleep disturbances and some common effects of sleep deprivation.

Mitochondrial Dysfunction
Mitochondria, often described as the cell’s “batteries,” are crucial for providing energy (ATP) to every cell in the body. Their dysfunction has been notably linked to chronic fatigue syndrome (CFS), particularly in differentiating “post-exertional malaise” seen in ME/CFS from general burnout or tiredness. In cases of ME/CFS, rest alone often doesn’t restore energy (Booth et al., 2012).
Recent advancements in mitochondrial science have expanded our understanding of their role. Beyond energy generation, mitochondria are integral to overall health, with functions including hormone and melatonin production, antioxidant synthesis, regulation of cell death and cancer processes, aging, and immune system/inflammation management.
Given this broad scope of influence, it’s unsurprising that mitochondrial dysfunction is implicated in a wide array of chronic health conditions, including:
Cancer (Hanahan, 2011)
Neurodegenerative disease like Parkinsons and Alzheimer’s (Compagnoni 2020)
Type 2 diabetes/insulin resistance and obesity (Yuzefovych, 2019)
Cardiovascular disease (Poznyak et al., 2020)
Fibromyalgia (Cordero et al., 2010)
and Autism (Siddiqui et al., 2016).
This dysfunction may explain why these conditions frequently cluster in family lineages, particularly along maternal lines, as mitochondria are inherited maternally. This inheritance pattern can lead to higher ratios of conditions like CFS, Fibromyalgia, and certain autoimmune diseases in females. In Functional Medicine, we delve into these associations and utilize therapeutic tools to address specific mitochondrial dysfunctions.
IBS (Irritable Bowel Syndrome) and Its Intersection with CFS/ME and Autism
IBS is frequently seen within the context of CFS/ME, with an estimated 30-90% overlap, and autism, where Autistic children are four times more likely to experience gut issues (McElhanon et al., 2014). IBS is often a diagnosis of exclusion, meaning, the diagnosis is used when a range of gut and digestive symptoms cannot be explained by objective medical tests.
The Gut-Brain Axis
The bi-directional relationship between the gut and the brain, primarily through the vagus nerve, offers a holistic view of how emotions can affect gut function and vice versa. This connection is crucial in understanding the interplay between mood, cognition, and gut health. A large Randomized Controlled Trial (RCT) demonstrated that gut-directed hypnotherapy positively influenced both physical and psychological symptoms in IBS patients and was even more effective than a low-FODMAP diet for psychological symptoms (Peters et al., 2016).
Interoception, Insular Dysfunction, and IBS
Both impaired interoception and insular dysfunction (a disruption in the brain region involved in emotional and sensory processing), prevalent in Autistic individuals, are also central to IBS. These factors can influence gut function in various ways (Bonaz et al., 2021), including:
Increased sensitivity to digestive pain.
Heightened reactions to ingested substances unrelated to the immune system (e.g., non-allergic food sensitivities).
Abnormal sensory processing of food characteristics.
Challenges in regulating appetite, satiety, toileting needs, or thirst.
Emotional or stress responses manifesting as hunger, fullness, stomach aches, or bloating.
Elevated markers of digestive and neuro-inflammation.
Gut Inflammation and IBD: Links to CFS/ME and Autism
Inflammatory bowel diseases (IBD), such as Crohn’s Disease and Ulcerative Colitis, have a notable connection with Chronic Fatigue Syndrome (CFS/ME). Individuals with IBD are at an increased risk of developing CFS/ME (Tsai et al. 2019). Similarly, substantial research in Autistic children has linked their gut symptoms to underlying inflammatory bowel conditions (Lee, 2018).
The Gut-Brain Connection and Mood Disorders:
There is robust evidence that mood disorders, including depression, anxiety, and fatigue, are associated with inflammation and immune system activation (Lee, 2018). This link further underscores the critical gut-brain connection and opens promising avenues for support and investigative options for people experiencing fatigue and mood challenges, regardless of either a diagnosis of CFS/ME or autism.
Gut Dysbiosis & Parasites: Impacts on Immunity and Chronic Conditions
Our gut houses 70-80% of the immune system, making the balance of gut bacteria critical for immune function and metabolic health. Dysbiosis, an imbalance between beneficial and harmful gut bacteria, has been a focal point in understanding the link between diet, gut health, and various chronic conditions, including Long-COVID (UCLA article 2021).
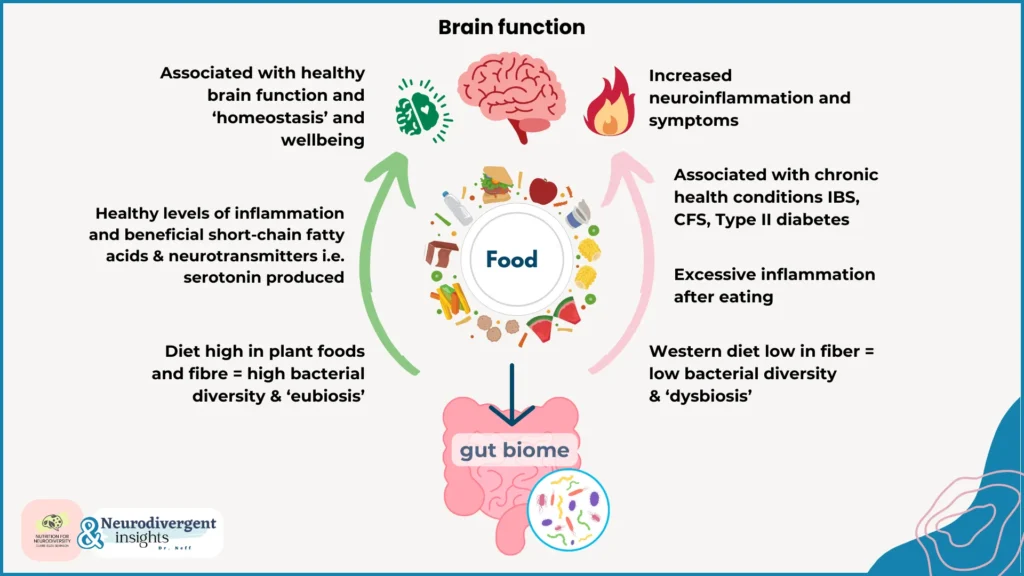
Large-scale studies, such as ZOE, have shown that fiber-rich diets increase microbial diversity and the presence of key species that produce anti-inflammatory and immune-boosting chemicals. This can lead to a healthier gut environment, reduced gastrointestinal complaints, and improved physical and mental health outcomes. It also positively influences metabolic responses to food, like blood sugar regulation, helping to prevent conditions like type II diabetes (ZOE, 2023).
Research on the gut microbiome in CFS/ME patients, particularly regarding neurological and mood symptoms, has found reduced microbial diversity, higher amounts of pro-inflammatory species, and fewer anti-inflammatory bacteria (Giloteaux et al., 2016).
In the context of autism, reduced microbial diversity has long been associated with gastrointestinal issues. Innovative treatments, such as Fecal Microbial Transplant (FMT), have been explored. In a clinical trial, Autistic participants (with significant support needs) receiving FMT showed improvements in motor skills, GI symptoms, and a variety of behavioral aspects up to two years post-treatment (Kang et al., 2019). However, the exact link between the gut microbiome and autism is still debated. Notably, studies like Yap et al. (2021) suggest that restricted eating patterns and dietary preferences common in autism might contribute to reduced microbial diversity and GI symptoms.
Gut Hyper-Permeability (Leaky Gut) and intestinal barrier dysfunction
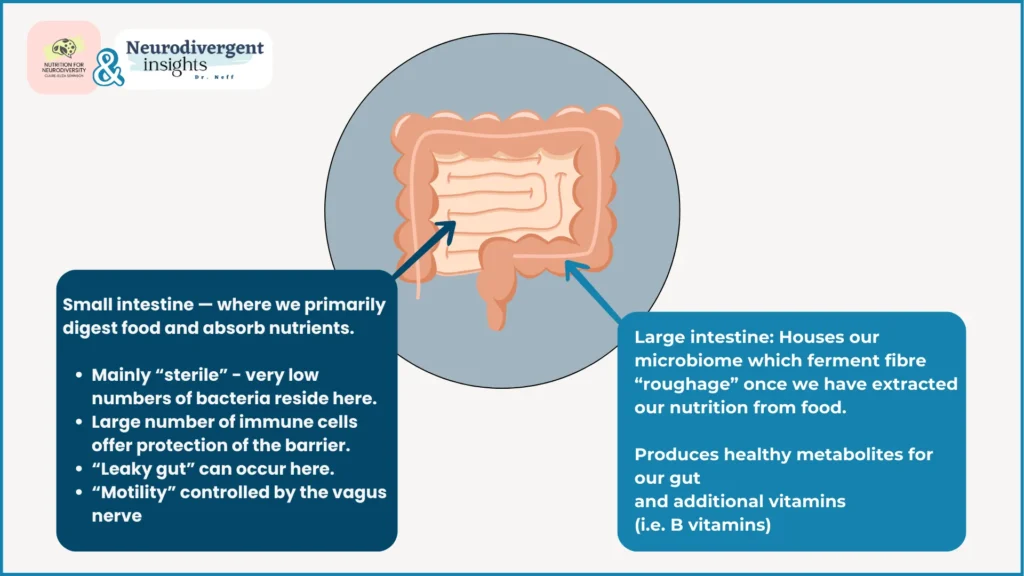
Our intestinal barrier is a complex barrier and our first line of defense against toxic substances we may ingest. It is made up of many types of functional cells held together by “tight junction proteins” – a bit like bricks in a wall held together by cement. The gut has to allow water and nutrients from our food into our bodies whilst keeping out the “bad guys” – pathogens such as bacteria, viruses and toxins. Immune cells like mast cells and lymphocytes are stationed close to this barrier to neutralize any potential threats.
What is Leaky Gut?
Gut hyper-permeability, or “leaky gut,” occurs when the gut barrier becomes more permeable than usual, allowing particles that don’t normally enter our bodies to pass through. This can be due to several factors, including autoimmune attacks on tight-junction proteins or inflammatory responses from infections. When substances like large food proteins or chemicals enter the bloodstream, the immune system recognizes them as foreign, and mount an attack as if it was a dangerous infection or an allergen resulting in inflammation and/or multiple food intolerances that can affect many systems in the body simultaneously.
Markers of leaky gut are linked with digestive issues, inflammatory bowel conditions, food allergies, and related disorders like eczema or asthma. However, it’s still debated whether leaky gut is a cause or an effect of these conditions.
Leaky Gut and Chronic Fatigue Syndrome
In CFS, leaky gut has been correlated with illness severity, cognitive difficulties, muscle tension, and irritable bowel (Maes, 2007). A notable study by Maes and colleagues found that addressing weakened gut barriers and dysbiosis in CFS patients led to significant improvements or complete remission of symptoms.
Leaky Gut in Autism
Likewise leaky gut is also implicated in Autistic people. One study found 36.7% of Autistic children had higher intestinal permeability compared to less than 5% of allistic children. Autistic people also have higher rates of food intolerances, allergies and multiple chemical sensitivities all of which are complications that arise from intestinal barrier dysfunction.(Dargenio, et al., 2023)
The take home message is gut issues coexist with autism and CFS in complex ways. Research demonstrates bi-directional mechanisms between the gut and the brain. Whilst it is unlikely to cause either condition, much of the symptoms associated with distress, suffering, fatigue, pain and IBS could be alleviated and modified when examining these links.
SIBO & Gut Motility Issues
Small intestinal bacterial overgrowth, or SIBO, is a condition detected in up to 80% of people with IBS and is also associated with a wide range of chronic conditions, including CFS and autism.
Understanding SIBO
SIBO occurs when bacteria, typically found in the large intestine, overgrow in the small intestine – the primary site for digestion and nutrient absorption. This overgrowth leads to bacteria fermenting food, producing gases like hydrogen and methane, and other byproducts like histamine. The result can include upper digestive symptoms such as bloating, pain, cramping, diarrhea, or constipation, along with widespread inflammation and various body and brain symptoms.
Symptoms often appear within 90 minutes of eating, especially after consuming high FODMAP foods that bacteria readily ferment, like onions, cauliflower, chickpeas, lentils, and garlic.
Consequences of SIBO
The inflammation from SIBO can lead to malabsorption and nutritional deficiencies. For instance, iron deficiency anemia is common among those affected.
Complexities in SIBO Development and Treatment:
Understanding and treating SIBO is complex, and the condition is known for being difficult to manage and prone to recurrence. Our current understanding suggests that SIBO is a motility disorder. The autonomic nervous system controls peristalsis (contractions moving food through the digestive tract) and the migrating motor complex (MMC), which are critical for preventing bacterial buildup in the small intestine. These processes are regulated by the vagus nerve, and any impairment in vagal motor outflow can lead to disorders like SIBO and constipation.
Psychological stress, anxiety, and trauma, known to affect vagal tone, are also believed to play a role in SIBO, particularly in cases that are recurrent or resistant to treatment.
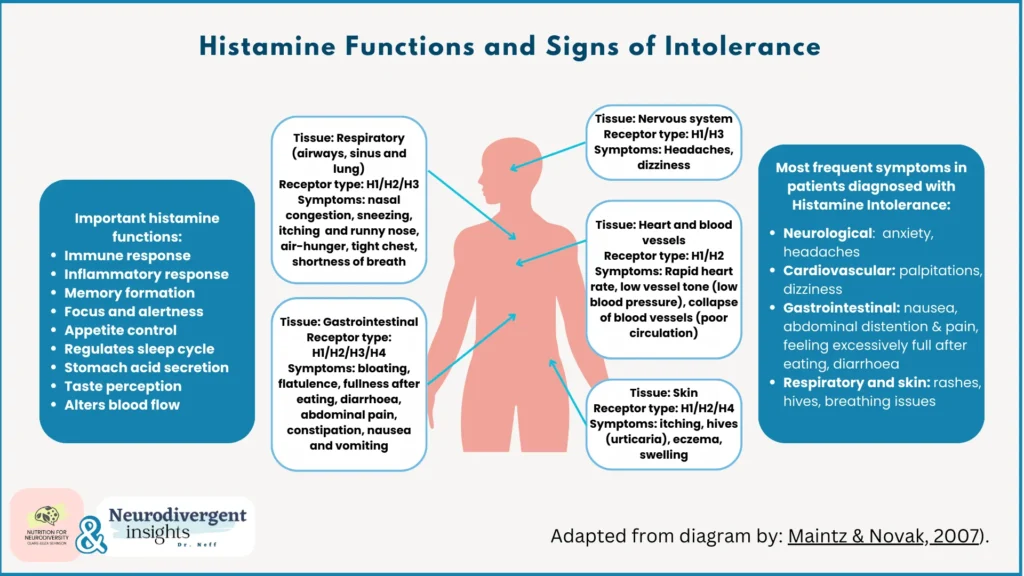
Mast Cell Activation & Histamine Intolerance
Histamine, a key chemical and neurotransmitter, plays diverse roles in our immune, digestive, cardiovascular, and nervous systems. Histamine intolerance (HIT) occurs when the body’s capacity to break down histamine is compromised, leading to an accumulation. Due to the wide distribution of histamine receptors, HIT can cause a variety of symptoms throughout the body such as:
Skin Reactions: Including hives, itching, and rashes.
Digestive Issues: Such as diarrhea, nausea, vomiting, and abdominal cramps.
Respiratory Problems: Including nasal congestion, sneezing, asthma, and difficulty breathing.
Neurological Symptoms: Such as headaches, migraines, dizziness, and fatigue.
Cardiovascular Effects: Like irregular heartbeats, blood pressure changes, and flushing.
Mental Health Impacts: Including anxiety, difficulty sleeping, and irritability.
Allergic Reactions: Ranging from mild sensitivities to severe allergies.
(Reference: Maintz & Novak, 2007).
Histamine Intolerance (HIT)
Histamine Intolerance (HIT) occurs when the body struggles to break down histamine efficiently. This condition can arise from a deficiency in histamine-degrading enzymes:
Diamine Oxidase (DAO): This enzyme is found in the mucosal linings of the gut, lungs, and uterus.
Histamine N-Methyl-Transferase (HNMT): This enzyme works inside our cells.
These deficiencies might be genetic or stem from other issues like inflammatory bowel disease or leaky gut, which reduces DAO’s available surface area. Additionally, menopause can significantly decrease DAO production in the uterus.
External Sources of Histamine
Histamine can also be produced by some strains of gut bacteria and is present in a large number of foods in our diet – both of which can add to the bucket load.
Hormones and Histamine
Oestrogen and xenoestrogens (natural or synthetic chemicals that mimic estrogens in the body) are also found to lower DAO and trigger mast cells to release histamine. The natural ebb and flow of hormones during the menstrual cycle can add additional histamine challenges at different times.
*** Clinically we observe that some patient’s will notice their HIT symptoms get worse around certain points in their cycle or the period where they first experienced HIT may coincide with peri-menopause.
Mast Cell Activation
Histamine and various other chemicals are stored and released from mast cells. Mast cells are part of our first line immune response. They also act as sensors of stress and danger being strategically positioned or surfaces that interface the “outside world” such as our skin, gut lining, airways and the blood-brain-barrier so that any pathogens are dealt with before they have a chance to enter.
What is also intriguing is that mast cells release a hormone called Corticotropin Releasing Hormone which induces the production of cortisol from the adrenal gland. So mast cells induce stress but stress and fear in turn activate mast cells in a vicious cycle. This association was described by Theoharides and his group in Autistic children.
Mast Cell Triggers
Mast cells can be activated by various factors, including allergens, infections, certain drugs and medications, hormones, endorphins, toxic metals, IgE/G antibodies, histamine-rich foods, and physical stress (i.e. exertion from strenuous exercise or cold/heat stress or sudden temperature changes).
Mast cells develop a ‘metabolic memory,’ becoming more sensitized and reactive over time. Mast Cell Activation Syndrome (MCAS) occurs when mast cells become unstable and are easily triggered, often requiring minimal stimulation.
MCAS and HIT
Approximately 20% of people with histamine intolerance will also have MCAS, however they are not the same condition and working with MCAS is a more complex process. MCAS is one of thefeatures of immune dysfunctionand is believed to play a role in Long-COVID andME/CFS.
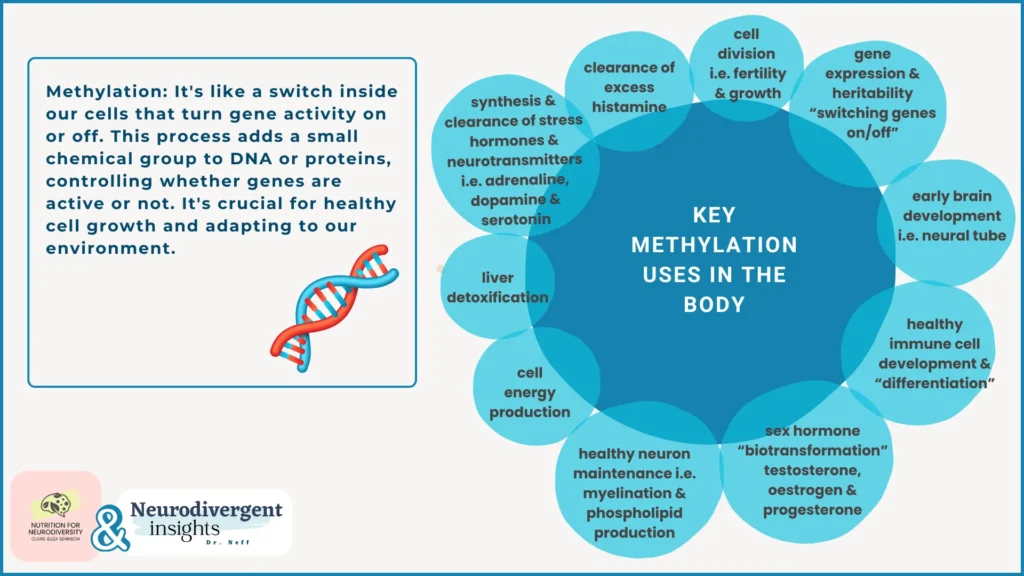
Methylation (Epigenetics and Genomic SNPS)
The Role of Methylation in Cellular Function
Methylation, a critical biochemical process in every cell, has profound implications in various health conditions. It has long been discussed in health research including autism, heart disease, cancer, hormone imbalances, fertility, and chronic illnesses.
Epigenetics and Methylation
One of the most pivotal roles of methylation is in epigenetics – the study of how gene expression is regulated by external and environmental factors without altering the DNA sequence. Methylation acts as a molecular switch that can turn genes on or off, a process crucial for normal development and cellular differentiation. This means that while our DNA provides the blueprint, methylation patterns determine how, when, and to what extent these instructions are used.
One of the landmark studies to demonstrate this was the Dutch Hunger Winter study. Pregnant people exposed to famine and stress during this period had descendants, even multiple generations later, with higher rates of metabolic conditions (cardiovascular disease, diabetes), neurodegenerative diseases, poorer cognitive function, increased breast cancer risk, overall cancer mortality, and symptoms of anxiety and depression.
Furthermore, Dr. Moshe Syzf’s research in “social epigenetics” explores how early life adversity and trauma can be inherited intergenerationally through DNA methylation.
Methylation, SNPs, and Personalized Health
Methylation’s role in health is further complicated by genetic variations known as single nucleotide polymorphisms (SNPs). Variations in genes involved in the methylation process can influence how effectively these mechanisms work, potentially predisposing individuals to various health conditions.
Autistic people and CFS patients (as well as host of other chronic health conditions) are found to have higher methylation deficits due to variations of some key methylation genes such as the MTHFR (methylenetetrahydrofolate reductase) 677T gene. These genes express “methylation enzymes” that perform these chemical reactions. So having variations in these genes means methylation processes in the body can run more slowly than usual.
Our methylation capacity depends on key nutrients such as folate, B12, B6 and betaine, all of which can be obtained from our diet. However the MTHFR 677T snp (associated with chronic health issues) means these nutrients cannot be “activated” to the form needed in our cells.
Importantly methylation is a key area of excitement for practitioners due to available nutrigenomic testing and dietary, lifestyle and supplement protocols that can be applied. However we caution with over-supplementation or self-prescribing as methylation requires balance and many people’s experience of using active or high strength supplementation is a worsening of their symptoms as over-methylation can have negative consequences too. So it is always advisable to work with a functional medicine or nutritional therapy practitioner for personalized guidance.
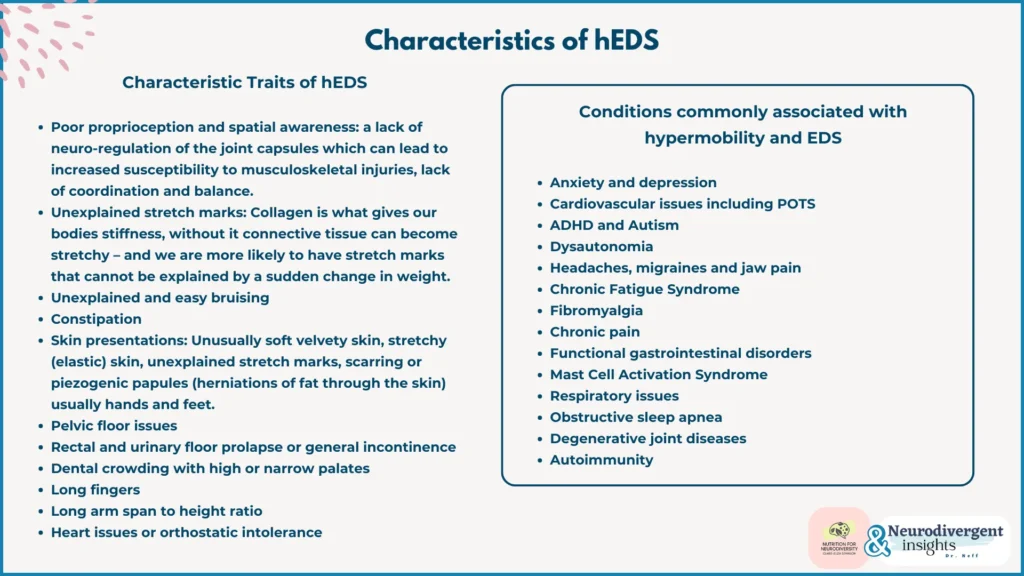
Understanding Hypermobility
Having joint hypermobility(often referred to as being “double-jointed”) means that your joints have a larger than normal range of movement due to the laxity of the ligaments and structures of the joint capsule. This increased movement, can lead to instability. People can be hypermobile in just one joint or multiple joints around the body (and there are over 350 in the human body!)
Hypermobility is often a genetic predisposition but it can also occur following trauma or injury (i.e. a dislocated shoulder) or secondary to a connective tissue disorder or autoimmune condition such as Lupus.
Ehlers Danlos Syndrome
EDS encompasses a group of inherited connective tissue disorders, with 13 known subtypes. Most are marked by varying degrees of joint hypermobility, with hypermobile EDS (hEDS) being the most common. This involves an inherited issue with collagen production, the most abundant protein in the body. Collagen is vital for providing strength and support in the musculoskeletal system and adds ‘stiffness’ to structural tissues.
This stiffness gives integrity to structures such as our gut (in order for us to have normal motility and bowel transition) and our arteries (in order for us to keep our blood pressure up and pump blood to our brain). Our eyes, skin, heart valves and uterine lining are all composed of collagen too. So when we have a collagen disorder, we can experience a wide array of symptoms.
Hypermobility in CFS and Fibromyalgia
Studies indicate that up to 81% of individuals with CFS and Fibromyalgia meet criteria for hypermobility syndromes (Eccles et al., 2021). Additionally, people with EDS are significantly more likely to be Autistic (7 times) and to have ADHD (6 times) compared to the general population (Csecs., et al 2022).
Brain Imaging Studies
Compelling brain imaging studies found that people with hypermobility often have larger fear processing centers in the brain. This finding aligns with the prevalent mental health conditions observed in both Autistic and CFS populations, highlighting a potential neurological basis for these overlapping experiences.
Dysautonomia and POTS (Postural Orthostatic Tachycardia Syndrome)
Understanding Dysautonomia
Dysautonomia is the inability of your autonomic nervous system to regulate itself, which includes involuntary functions such as blood pressure, heart rate, body temperature, blood sugar levels or breathing patterns. With dysautonomia the communication between your autonomic nervous system and the rest of your body is out of sync which results in great difficulties in adapting to or regulating yourself for example if the room temperature changes, adjusting from sitting to standing positions or energy levels if you haven’t eaten anything for a few hours. The effects can range from mild to severe.
Dysautonomia can be hereditary (rare) or develop secondary to other health issues, including neurodegenerative diseases (like Parkinson’s), central nervous system infections (such as CMV, Lyme, and COVID), traumatic brain injury, autoimmune disorders (like M.S., Lupus), vitamin B1 or B12 deficiencies, Ehlers Danlos Syndrome, mitochondrial diseases, and many more.
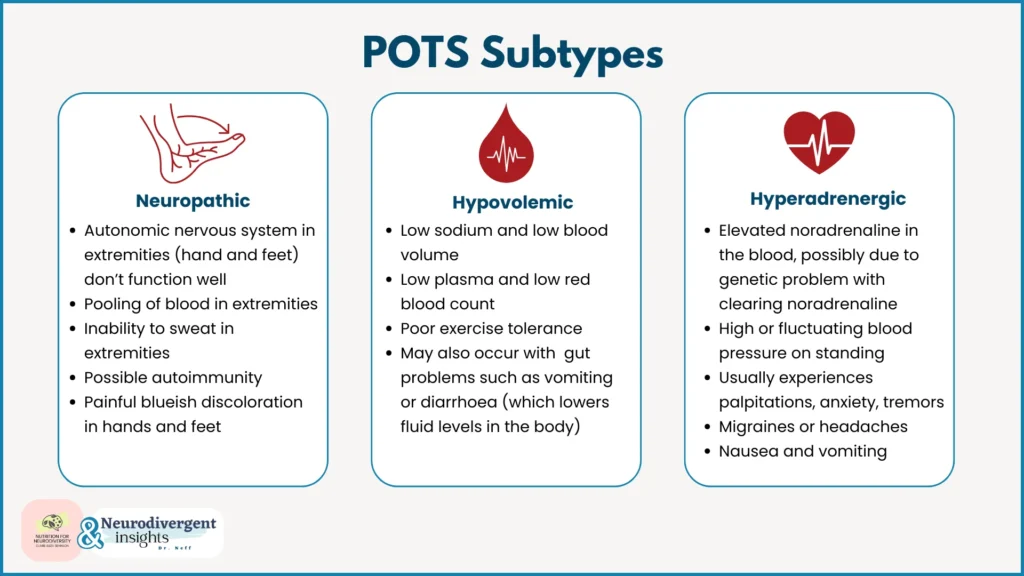
POTS: A Common Form of Dysautonomia
POTS (postural orthostatic tachycardia syndrome), one of the most prevalent types of dysautonomia, is often identified by a rapid increase in heart rate upon standing, accompanied by symptoms like dizziness, a “head rush,” or fatigue.
Mechanism Behind POTS
In POTS, the autonomic nervous system struggles to adapt quickly enough when moving from sitting or lying down to a standing position. Normally, blood vessels need to contract swiftly to send blood and oxygen to the brain. However, in POTS, this response is delayed, making the heart work harder to pump blood upwards, resulting in tachycardia (rapid heart rate) or symptoms like faintness, dizziness, or fatigue due to reduced oxygen flow.
POTS in CFS, Chronic Illness, and Autism
POTS is commonly observed in individuals with CFS, chronic illnesses, and Autistic people. Management often includes increasing salt and fluid intake to boost blood volume. Functional medicine practitioners also seek to identify and address underlying causes, which can range from supporting hypermobility issues to resolving infections affecting cranial nerves, to improve autonomic nervous system function.
Insufficient Vitamin D, Essential Fatty Acids & Minerals
Nutritional Deficiencies in Autism and CFS
Autistic and CFS patients often exhibit nutritional deficiencies or sub-optimal levels of vital nutrients. Common deficiencies include vitamins (D, folate, B12, and C), long-chain omega fatty acids (EPA & DHA), and minerals (zinc, iron, magnesium).
Causes of Vitamin Insufficiencies:
These vitamin insufficiencies can have multiple causes:
Autoimmune Gut Conditions: For instance, pernicious anemia where the immune system attacks cells that produce a protein called ‘intrinsic factor’ that binds to vitamin B12 so it can be absorbed. Without intrinsic factor we see low B12 and this can lead to anemia.
Digestive Issues and Malabsorption: Clinical observations often reveal low stomach acid, crucial for mineral absorption such as zinc, magnesium and iron. Additionally, leaky gut can impede nutrient absorption due to damage to mucosal surface transporters.
Restrictive eating patterns: Sensory difficulties, ARFID or eating disorders can impact the range of foods eaten and this reduces the variety of nutrients the person is able to obtain from their diet
Geographical Factors: Vitamin D from sunlight is inadequate in many regions north of the equator. An easy way to tell is the vitamin D shadow rule.
Genetic Factors: Variations like MTHFR can affect folate activation.
Mineral Status and Vitamin D: Low vitamin D levels can impact calcium and magnesium absorption.
Modern Agriculture: Modern farming methods and soil depletion reduces the nutrient density of foods, particularly selenium and magnesium.
Essential Fatty Acids: Omegas 3,6,9 are much lower in the modern diet with higher processed foods and lower whole-foods. Fat malabsorption disorders can hinder fat-soluble vitamin absorption (i.e. vitamin D or A) even if the person is eating sufficient amounts. Viral infections can additionally impair our ability to make long-chain fatty acids.
Vegan diets: Vegan diets are typically low in iron and B12 and may require supplementation
Heavy menstruation: Heavy menstration can results in iron loss.
Chronic infections: Bacteria and fungal infections utilize iron for their own metabolism
Chronic stress: Stress can lower stomach acid, reroute nutrients like zinc and vitamin C to support the stress response, and detract from other bodily functions.
Dietary factors: High sugar consumption can deplete vitamin C, while diuretics like caffeine or alcohol increase the loss of B vitamins, electrolytes, and minerals.
Hypothalamic-Pituitary-Adrenal (HPA) Axis Dysfunction
The HPA-Axis refers to the complex neuro-endocrine feedback loop between the hypothalamus and pituitary (in the brain) and the adrenal glands that sit above our kidneys.This system orchestrates the body’s response to stress.
Stress Response Mechanism:
During physiological and psychological stress “fight-flight-freeze”, the hypothalamus releases corticotropin-releasing hormone, stimulating the adrenal cortex to release cortisol and DHEA. These hormones prepare the body for “survival” by increasing energy availability to our muscles and brain, whilst shutting down non-essential processes like digestion and the immune system.
The adrenal glands also produce catecholamines (adrenaline, noradrenaline, and dopamine), which drive the “reflex reactions” in acute stress situations.
Short periods of adrenal stimulation favors survival in immediate danger or threat. However, prolonged and persistent stimulation of the stress response is demonstrated to play a role in the development of a multitude of metabolic disorders as well as CFS, cognitive decline, burnout and the majority of chronic illnesses (Tomas et al., 2013).
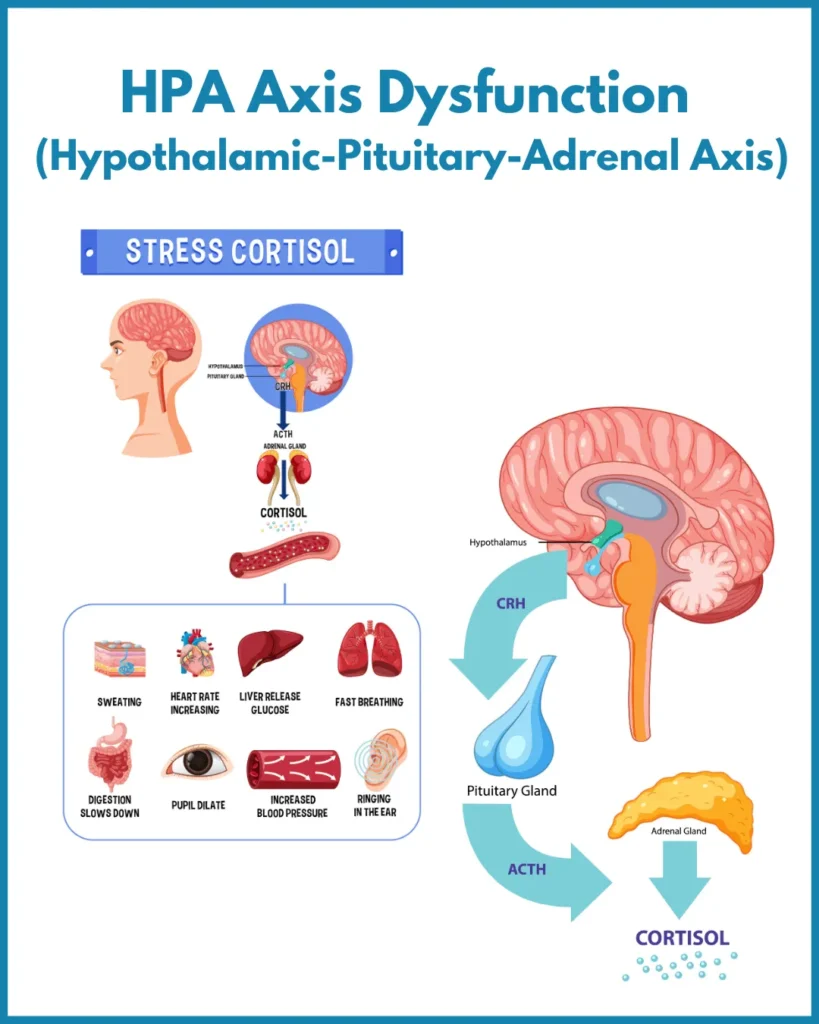
HPA Axis Dysfunction in Chronic Fatigue:
Research consistently describes a state of HPA axis dysfunction in people with chronic fatigue and this shows up as:
A disruption of circadian rhythm – that can affect waking energy and getting to sleep
Reduced cortisol output in the long run because cortisol receptors in the brain become overly sensitized to cortisol and reduce cortisol output (“negative feedback loop”) – clients with this pattern tend to describe and loss of resilience and a “tired-but-wired” feeling like they are running on adrenaline
In particular a blunted morning surge of cortisol – clinically this looks like a person who lacks the “get up and go” and feels completely exhausted
*HPA axis dysfunction is also more prevalent in females
Autistic children and adults have highly sensitive nervous systems and many types of social and sensory input can be experienced as overwhelming, unpleasant or even threatening. Our nervous system can go into fight-flight-freeze with alarming regularity to seemingly “nothing”. This chronic stress activation has been demonstrated to result in HPA axis dysfunction with consequences such as poor immune function and inflammation (Makris et al., 2021).
Chronic Hypervigilance “Limbic Kindling”
In this context, the nervous system’s response to perceived threats can become exaggerated over time, a phenomenon known as “limbic kindling.” The limbic system (part of our brain responsible for survival, fear, emotions and memory) can become “hard-wired” to react to perceived threats more easily, even if the original threat is no-longer there. This means that the HPA axis is altered in a way that less stimulus is needed to trigger a state of hypervigilence (Gelhorn, 1970). This heightened state of alertness can further exacerbate HPA axis dysfunction and its associated health impacts.**
Hypersensitization in CFS/ME
This heightened sensitivity to stimuli, whether chemical, infectious, or psychological, has been observed in CFS/ME patients (Gupta, 2002). Limbic kindling can significantly affect the health of individuals with CFS, leading to a variety of issues. As outlined by Jason et al., 2011, limbic kindling in CFS can lead to:
Imbalances in the immune system.
Increased allergic reactions.
More frequent chronic infections.
Reduced brain volume.
Lower levels of GABA and acetylcholine, crucial neurotransmitters for the parasympathetic nervous system, which plays a key role in relaxation and recovery.
Neuroinflammation in ME/CFS and Autism
Neuroinflammation in ME/CFS:
Many of the core symptoms of ME/CFS, such as brain fog, fatigue, pain, and sensory sensitivities, are linked to neuroinflammation. The brain’s immune cells, known as microglia, play a central role in this process. When microglia detect that something is wrong, like presence of pathogens, low oxygen levels, or inflammation in other body parts (like the gut), they become activated. This activation leads to the production of inflammatory and excitatory chemicals, such as glutamate, heightening nerve signaling in the brain. This can manifest as increased sensitivity and difficulty concentrating. Neuroimaging studies of CFS patients, such as Nakatomi et al. (2014), have identified neuroinflammation in critical brain areas related to pain processing, brain stem function (including the vagus nerve), and autonomic processing (which regulates heart rate, respiratory rate, and reflexes).
Neuroinflammation in Autism
Similar patterns of neuroinflammation and microglial activation have been consistently observed in Autistic children (Tsilioni et al., 2019). Autistic research often focuses on the connection between neuroinflammation and social behaviors, communication difficulties, and the atypical wiring of the limbic system. However, insights from neuroinflammation research in CFS and other chronic illnesses offer valuable perspectives. By understanding and addressing neuroinflammation, it may be possible to alleviate symptoms like pain, sensory overload, and hypervigilance, leading to reduced distress behaviors in Autistic individuals.
Understanding Low Vagal Tone
The Vagus Nerve: A Key Component in the Body-Brain Communication
The vagus nerve, or the 10th cranial nerve, originates from the brainstem and connects to most major organs. It’s aptly named “Vagus” (Latin for ‘wandering’)as it connects to all of your major organs. The communication via the vagus nerve is bi-directional, allowing signals to travel both from the brain to the body and vice versa. Interestingly, the majority (about 80%) of this neural communication is from the body to the brain. The vagus nerve is the main nerve that innervates the gut – and is what we refer to when we talk about the gut-brain-axis.
Role of the Vagus Nerve
As the dominant nerve of the parasympathetic nervous system, the vagus nerve plays a role various conditions, including depression, PTSD, immune dysfunction, autoimmunity, pain, epilepsy, cardiovascular disease, cognitive decline, autism, ADHD, fibromyalgia, tinnitus, sleep issues, aging, and more.
Vagal Tone
The vagus can have high or low “tone” describing the fitness of this nerve. Good vagal tone is associated with a range of positive health outcomes, including a longer lifespan, reduced stress and pain, and improved mood. Conversely, poor vagal tone is linked with stress-related chronic illnesses, digestive issues (like constipation), sleep disorders, heart disease, and depression (Bonas et al., 2016; Bonaz et al., 2017).
Low Vagal Tone in Autism and CFS
Poor vagal tone has long been observed in Autistic and CFS populations, indicating less flexibility in their nervous systems. For Autistic people this might result in stress easily induced by social encounters, sensory input, routine disruption, unexpected changes, and difficulties with emotional regulation.
With CFS, as vagal tone declines over a lifetime people tend to find their resilience to any environmental stimuli or interpersonal triggers decrease and they become more reactive to everything. These experiences echo the sensory overload and emotional dysregulation often experienced by Autistic people from birth and low vagal tone is one of the overlapping factors.
Electrical Stimulation for Vagal Tone Improvement
Encouragingly, there are many ways to improve vagal tone. Through lifetime modifications, limbic retraining and vagal nerve stimulators. Studies exploring electrical stimulation, like using a TENS machine, have shown promise in improving symptoms of chronic fatigue and fibromyalgia. For instance, Traianos et al. (2021) demonstrated symptom improvement in CFS and fibromyalgia patients through non-invasive electrical stimulation.
Food and Chemical Sensitivities in Autism and CFS
The majority of Autistic individuals and CFS patients report sensitivities to multiple foods and chemicals. They can produce an array of bewildering and worrying symptoms affecting the whole body for prolonged periods of time – so it is important to distinguish what they are in order for them to be managed properly.
Clinically these reactions can be broken down into types.
Immunological Reactions: These include immune-based reactions like allergies, intolerances, or mast-cell activation. Mediated by antibodies (IgE, IgG), inflammatory cascades, or histamine levels, these reactions often have common triggers due to overlapping proteins. For example, birch pollens and related fruits like apples, almonds, peaches, and cherries. Leaky gut syndrome can also lead to large food proteins entering the bloodstream, linking to autoimmune gut disorders (such as Celiac or Crohn’s disease) or atopic conditions (eczema, asthma, hayfever).
Interoceptive Sensitivities: These involve sensitization to the characteristics of food or chemicals, such as texture, taste, odor, temperature, eating environment, or associations with specific memories (e.g., choking, vomiting, food poisoning). This type often presents as IBS, with stomach upsets being a common manifestation of stress and overload. The enteric nervous system (nervous system that innervates the entire digestive tract) plays a significant role here. Antibody tests typically show no abnormalities, and the condition is not linked to inflammation. Unlike immunological reactions, interoceptive sensitivities vary widely and relate to individual sensory preferences and aversions. Addressing these sensitivities, especially in conditions like ARFID (avoidant restrictive food intake disorder) and non-inflammatory IBS, requires a nuanced understanding of interoception and fostering a safe environment around food in a Neurodivergent-affirmative way.
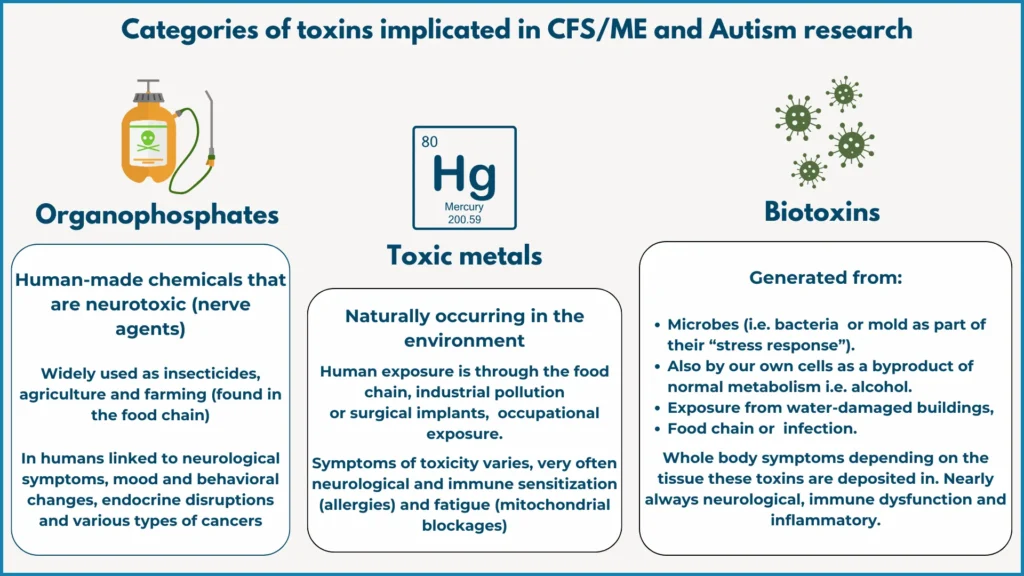
Toxicity and Its Impact
Understanding Toxicity
The concept of toxicity in mainstream research lacks a clear consensus. Toxicological studies looking at safety upper limits of chemicals focus on how much of a single toxin is required to cause harm in living organisms. In reality, toxin exposure does not work like this. We have low level exposure to thousands of toxins simultaneously (at levels that have been considered “safe”) and this multiplicity in exposure can overwhelm our capacity to excrete them.
A landmark investigation by the Environmental Working Group looked at the body burden of chemicals, pollutants and pesticides in the umbilical cord blood of newborn babies and found an average of 200 chemicals, including 217 toxic to the brain and nervous system or carcinogens. This combined effect of multiple environmental pollutants has not been studied in human trials.
Clinical Observations and Functional Medicine Approach
Clinically, we see how accumulated toxic exposures over a lifetime can surpass the body’s detoxification capabilities. These toxins, deposited in tissues, can disrupt biological processes and lead to symptoms of toxicity. In functional medicine, the focus is on the intersection of genetic vulnerability and lifestyle-based susceptibility to toxins, devising strategies to facilitate their safe excretion.
Clinically we see how accumulated toxic exposures over a lifetime eventually outweigh the person’s capacity to detoxify/remove these from the body. These circulating toxins get deposited into our tissues and can disrupt normal biological processes resulting in widespread symptoms of toxicity. Therefore in functional medicine, the focus is often on the intersection between genetic vulnerability and lifestyle-based susceptibility of being exposed to certain types of toxins and working out how to facilitate the excretion of these toxins safely through nutritional, lifestyle or supplemental strategies.
There have been some key toxins associated with Autism and CFS, including:
Toxic metals: nickel, lead, mercury (Wojcik, 2006; Blazewicz et al., 2023; Yakob, 2006)
Organophosphates: Such as insecticides, DEET, glyphosate (Dunstan et al., 2005; Sagiv et al., 2018).
Biotoxins: Mold/mycotoxins (Brewer et al., 2013), viral and bacterial toxins (Morris et al., 2015).
Vulnerability to Toxicity
There are several factors influencing why some people are more vulnerable to toxicity and develop complex chronic illness, whilst others (including their partners and family members) may be exposed to the same toxins but do not become ill or symptomatic. Some factors include:
Genetic variants affecting detoxification capacity: Certain genetic variants can significantly influence the body’s ability to detoxify. For example, the GSTM1 gene typically encodes a protein essential for removing environmental pollutants and heavy metals from our cells. However, in some individuals, this gene may be reduced in function or deleted entirely – a condition known as GSTM1 deletion. This genetic alteration can lead to an accumulation of toxins in the body, a phenomenon known as “bioaccumulation.” This build-up of toxins due to impaired detoxification has been documented in studies by Nakanishi et al. (2022) and Aronica et al. (2022).
Nutritional deficiencies can exacerbate metal toxicity: Nutritional deficiencies, particularly in essential minerals like calcium, selenium, and zinc, can inadvertently increase the body’s absorption of toxic metals such as lead, mercury, and nickel. This happens because these toxic metals are structurally similar to essential minerals and compete for the same absorption pathways or transporters in the body.
When essential mineral levels are low, the body may mistakenly absorb more of these toxic metals. For example, in the absence of adequate calcium, lead can be deposited into bones, a site where calcium is normally found. In these bones, lead can disrupt normal functions, leading to various health issues. Similarly, deficiencies in selenium and zinc can lead to increased accumulation of other toxic metals in organs where these essential minerals are usually utilized.
Therefore, one effective strategy to reduce the risk of metal toxicity is to maintain adequate levels of essential minerals through a balanced diet or supplementation as needed. This approach helps ensure that the body preferentially absorbs and utilizes these beneficial minerals, reducing the likelihood of toxic metal accumulation.
The Impact of Digestive Function on Detoxification:Poor digestive function, particularly constipation, plays a significant role in the body’s detoxification process. The gut is a key player in eliminating toxins, largely due to its role in processing bile. Here’s how it works:
Bile and Toxin Elimination: The liver deposits most of the body’s toxins into bile. This bile, secreted by the gallbladder, then travels into the digestive tract.
Fiber’s Role: Once in the digestive tract, bile binds to dietary fiber. This binding is crucial because it allows toxins to be carried out of the body with the stool, effectively completing the detoxification process.
Constipation and Toxin Reabsorption: However, if constipation occurs, this process can be disrupted. Severe constipation can lead to a delay in excreting bile-bound toxins. When this happens, there’s a risk that these toxins can be reabsorbed back into the bloodstream instead of being excreted. This phenomenon, known as “entero-hepatic recirculation,” can lead to a buildup of toxins in the body.
Chronic Inflammatory Response Syndrome (CIRS): Chronic Inflammatory Response Syndrome (CIRS) is a condition identified in a significant portion of the population with chronic fatigue-like illnesses. A large DNA analyses of over 12,000 patients with chronic fatigue-like illnesses found that 24% of the population are unable to make antibodies to certain types of biotoxins/pathogens – such as mycotoxins (Shoemaker., 2014). The implications of this are significant. These individuals are unable to mount an effective immune response to neutralize and eliminate these toxins. Consequently, they tend to accumulate toxins in their bodies and experience exaggerated chronic inflammatory responses, even to minimal exposures. This results in a wide constellation of symptoms that most CFS and Autistic people will find familiar
Interestingly, this inability to produce specific antibodies is often linked to mutations in the HLA DR gene set. These genes have associations with numerous autoimmune conditions, suggesting a genetic predisposition to CIRS in certain individuals.
Further Reading
For a functional approach to understanding and managing toxicity see Dr. Jill Crista’s work on mold-related illness and Chronic Inflammatory Response Syndrome:
Toxic by Neil Nathan MD
Dr Jill Crista for mold related illness and CIRS (Chronic Inflammatory Response Syndrome)
Pyroluria
Overview and Prevalence
Pyroluria is a metabolic condition that can be either genetic or acquired, affecting up to 10% of the population. Notably, higher incidences of Pyroluria are seen in conditions like schizophrenia, OCD, social anxiety, substance misuse, the autistic spectrum, and CFS (McGinnis et al., 2008).
Discovery and Mechanism
Discovered in the 1950s by Dr. Abraham Hoffer and Dr. Carl Pfeiffer, Pyroluria involves the overproduction of kryptopyrroles, by-products of hemoglobin synthesis. Hemoglobin carries oxygen in our red blood cells, but kryptopyrroles themselves don’t serve any biological purpose and are typically harmless in small amounts. However, when produced excessively, they bind to zinc and vitamin B6, rendering these nutrients unavailable to tissues and cells. This binding leads to a loss of zinc and B6 through urine, a process that can be measured to diagnose Pyroluria.
Symptoms, Impacts And Clinical Approach
This depletion leads to chronic deficiency of zinc and B6 with the emergence of a myriad of wide-ranging symptoms. Zinc is crucial for over 300 bodily functions, especially in brain health, immune function, and stress response. Similarly, B6 is essential for neurotransmitter and hormone balance. Patients often describe a severe feeling of inner tension or poor stress tolerance.
It is believed that emotional trauma or stress can be a trigger to this process, but because zinc and B6 are such important nutrients for a healthy stress response, it then becomes more difficult for that person to bounce back from the episode and the vicious cycle continues. As a practitioner, pyroluria is something we try to identify early on because it is “treatable” with zinc/B6 repletion.
EMF Sensitivity: Understanding and Managing Exposure
What are Electromagnetic Fields (EMFs)?
EMFs are a combination of two naturally occurring invisible fields: magnetic (like the force between two magnets) and electrical (like the current flowing through a wire). In our bodies, our brain and nervous system use electrical currents to transmit information. EMFs occur where these electrical and magnetic forces combine.
Impact of Human-Made EMFs
Prolonged exposure to human-made EMFs, such as those from WiFi, can lead to hypersensitivities, particularly in vulnerable individuals. While research on safe exposure levels is ongoing, clinical observations often report EMF sensitivities in people with severe CFS and autism. Symptoms may diminish when exposure is minimized. The main biological effects and impacts on human health are outlined in the diagram below (Pall, 2018)
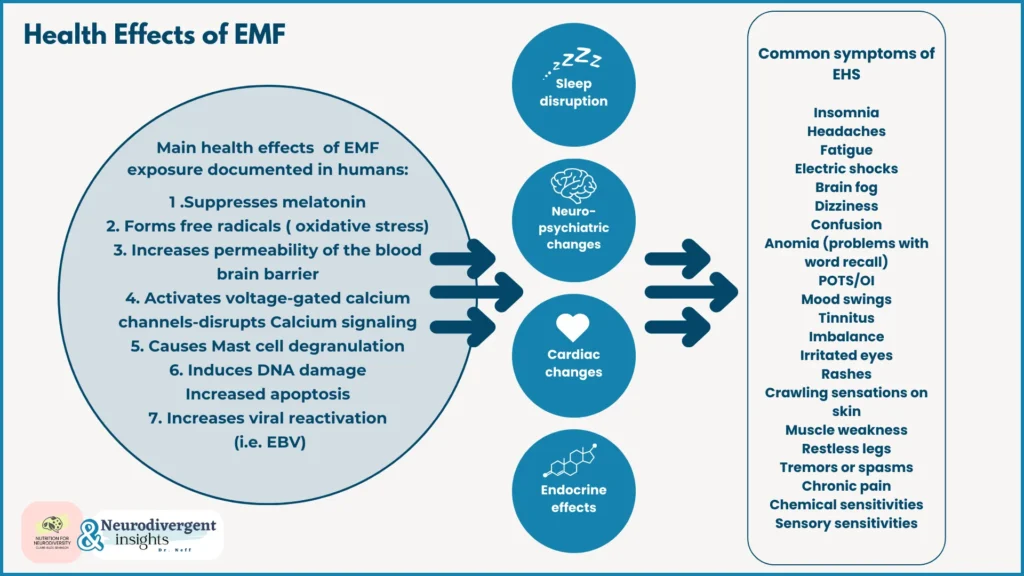
Biological Effects and Health Impacts
Some key mechanisms explaining symptoms seen in CFS/autism include:
Activation of Voltage-Gated Ion Channels: EMFs can activate “voltage-gated ion channels” on cell walls, particularly those of neurons. These channels function similarly to an electronic key card operating a door. When EMFs trigger these channels, they open, allowing calcium ions to flood into the cell. Calcium plays a crucial role as a signaling molecule inside our cells. For instance, in brain cells, this influx of calcium can initiate the release of neurotransmitters. In immune cells like mast cells, it can lead to the release of histamine and other chemicals. Consequently, EMF exposure can heighten various “sensitivities” due to these cellular responses.
Disruption of Melatonin Production: EMF disrupts melatonin production by the pineal gland and this has an obvious impact on sleep, but also inflammation (as melatonin has a huge anti-inflammatory impact on our cells) and antioxidant levels (again melatonin is one of our biggest antioxidant hormones that are protective to cell structures and our DNA).
Reactivation of Viruses: EMFs have been demonstrated to reactivate Epstein Barr Virus with as little as 50hz of EMF for 72 hours (Grimaldi et al., 1997). 50hz is considered low level exposure and is what most of us are exposed to daily (everyday electronic devices and power transmission lines).
Practical Tips for Managing EMF Sensitivity
For clients sensitive to EMFs, here are some top tips:
Double distance from the source (i.e. WiFi router or electrical outlet) it reduces exposure by 75%
Submerging in water is really helpful to calm symptoms. Taking an epsom salt bath in the evening can help with sleep disturbances and overstimulation
Use wired headphones with mobile phones (but not bluetooth)
Turn WiFi routers off overnight (especially if this is in close proximity to the bedroom)
Turn tech onto flight mode if sleeping with it nearby

Pain and Fibromyalgia in Neurodivergent Adults
Altered Pain Perception in Autism and ADHD
Autistic people and ADHDers often experience significant alterations in pain perception. They are more likely than neurotypical individuals to suffer from increased pain sensitivity, chronic widespread pain, and pain-related anxiety (Failla et al., 2020). One study found that 80% of adults with ADHD experience chronic widespread pain, compared to just 17% of neurotypical adults (Stray et al., 2013).
Understanding Fibromyalgia
Fibromyalgia is a chronic condition primarily characterized by widespread pain in connective tissues and muscles. Patients often experience a constellation of symptoms, including profound fatigue, anxiety, sleep disturbances, and cognitive challenges. While the precise cause of Fibromyalgia remains elusive, it is understood as an abnormality in how the brain processes pain signals. This abnormal processing can stem from various factors, including emotional trauma, genetic predispositions, or neuroinflammation. A key feature of Fibromyalgia is a heightened sensitivity to stimuli, leading to intensified pain experiences.
Fibromyalgia and Chronic Fatigue Syndrome (CFS)
There is a notable overlap between Fibromyalgia and Chronic Fatigue Syndrome (CFS). Research indicates that 30-55% of individuals diagnosed with CFS also meet the criteria for Fibromyalgia. Intriguingly, this comorbidity rate can rise to as high as 70% among patients with Fibromyalgia, suggesting a strong clinical and possibly pathophysiological connection between these two conditions (Afari and Buchwald, 2003).
Fibromyalgia and Neurodivergence
Recent research indicates a significant overlap between fibromyalgia and neurodivergence. For instance, a study screening 123 adults with fiibromyalgia for ADHD found that approximately 45% met the criteria for ADHD (van Rensburg, 2018). Research into pain mechanisms in neurodivergent individuals often points to centralized sensitization and neuroinflammation as underlying factors, paralleling findings in fibromyalgia studies.
Additionally, in clinical practice and research into Autistic children, it’s been observed that parents (especially mothers) of Autistic children frequently have diagnoses of CFS/ME or Fibromyalgia. Where testing was available, there were many shared heritable factors such as mitochondrial dysfunction (passed down the maternal lineage), shared genomics in inflammatory, histamine or methylation pathways and shared immune dysfunction. Given that autism has a 90% heritability rate it is highly likely that these conditions overlap. Considering the high heritability of autism, there’s a strong likelihood of overlap between these conditions.
It is our belief that a subset of individuals with CFS/ME and Fibromyalgia might represent a “lost generation” of undiagnosed Autistic and ADHD individuals, suggesting a deeper interconnectedness between these conditions and neurodivergence.
Conclusion
This article has delved into a range of complex and intertwined health conditions, with a special focus on the connections between autism, chronic fatigue syndrome (CFS), and other conditions commonly experienced alongside them.
We’ve examined key themes such as the impact of sleep disturbances, gut health issues, methylation and genetic factors, as well as the role of the HPA axis and vagal tone. The challenges posed by environmental factors like EMF sensitivity and mycotoxin exposure were also explored. Additionally, we delved into how dysautonomia, limbic kindling, and nutritional deficiencies crucially influence the manifestation and experience of these health conditions.
An important aspect that emerged is the concept of diagnostic overshadowing, where the presence of a well-known condition like autism or CFS can lead to the overlooking or misattributing of symptoms related to other co-occurring conditions. This highlights the need for a more comprehensive, nuanced approach to diagnosis and treatment.
This exploration underscores the necessity of recognizing individual differences and tailoring interventions to address the unique constellation of symptoms and underlying causes. As research continues to evolve and our understanding deepens, it is our hope that this article serves as a resource to shed light on these complex conditions and offer guidance for those navigating them, whether as patients, caregivers, or healthcare professionals. By embracing a comprehensive, empathetic approach to healthcare, we can better support those facing these often challenging and interwoven health journeys.
Further Learning
You can follow Claire’s work on Instagram and look forward to seeing more collaborative articles here on neurodivergent insights.
All The Things: Dr. Mel Houser’s website and work does a great job of highlighting hte intersection of neurodivergence and “all the things.” You can listen to them on our podcast, Divergent Conversations here.
References
Aaron RV, Fisher EA, de la Vega R, Lumley MA, Palermo TM. Alexithymia in individuals with chronic pain and its relation to pain intensity, physical interference, depression, and anxiety: a systematic review and meta-analysis. Pain. 2019 May;160(5):994-1006. doi: 10.1097/j.pain.0000000000001487. PMID: 31009416; PMCID: PMC6688175.
Afari, N., & Buchwald, D. (2003). Chronic fatigue syndrome: a review. American Journal of Psychiatry, 160(2), 221-236.
Aronica L, Ordovas JM, Volkov A, Lamb JJ, Stone PM, Minich D, Leary M, Class M, Metti D, Larson IA, Contractor N, Eck B, Bland JS. Genetic Biomarkers of Metabolic Detoxification for Personalized Lifestyle Medicine. Nutrients. 2022 Feb 11;14(4):768. doi: 10.3390/nu14040768. PMID: 35215417; PMCID: PMC8876337.
Acheson ED. The clinical syndrome variously called benign myalgic encephalomyelitis, Iceland disease and epidemic neuromyasthenia. Am J Med. 1959 Apr;26(4):569-95. doi: 10.1016/0002-9343(59)90280-3. PMID: 13637100.
Atchison CJ, Davies B, Cooper E, Lound A, Whitaker M, Hampshire A, Azor A, Donnelly CA, Chadeau-Hyam M, Cooke GS, Ward H, Elliott P. Long-term health impacts of COVID-19 among 242,712 adults in England. Nat Commun. 2023 Oct 24;14(1):6588. doi: 10.1038/s41467-023-41879-2. PMID: 37875536; PMCID: PMC10598213.
Bennett JA, Germani T, Haqq AM, Zwaigenbaum L. Autism spectrum disorder in Prader-Willi syndrome: A systematic review. Am J Med Genet A. 2015 Dec;167A(12):2936-44. doi: 10.1002/ajmg.a.37286. Epub 2015 Aug 29. PMID: 26331980.
Bested AC, Marshall LM. Review of Myalgic Encephalomyelitis/Chronic Fatigue Syndrome: an evidence-based approach to diagnosis and management by clinicians. Rev Environ Health. 2015;30(4):223-49. doi: 10.1515/reveh-2015-0026. PMID: 26613325.
Booth NE, Myhill S, McLaren-Howard J. Mitochondrial dysfunction and the pathophysiology of Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS). Int J Clin Exp Med. 2012;5(3):208-20. Epub 2012 Jun 15. PMID: 22837795; PMCID: PMC3403556.
Bonaz B, Sinniger V, Pellissier S. Anti-inflammatory properties of the vagus nerve: potential therapeutic implications of vagus nerve stimulation. J Physiol. 2016 Oct 15;594(20):5781-5790. doi: 10.1113/JP271539. Epub 2016 May 1. PMID: 27059884; PMCID: PMC5063949.
Bonaz B, Lane RD, Oshinsky ML, Kenny PJ, Sinha R, Mayer EA, Critchley HD. Diseases, Disorders, and Comorbidities of Interoception. Trends Neurosci. 2021 Jan;44(1):39-51. doi: 10.1016/j.tins.2020.09.009. PMID: 33378656.
Bonaz B, Sinniger V, Pellissier S. The Vagus Nerve in the Neuro-Immune Axis: Implications in the Pathology of the Gastrointestinal Tract. Front Immunol. 2017 Nov 2;8:1452. doi: 10.3389/fimmu.2017.01452. PMID: 29163522; PMCID: PMC5673632.
Brewer JH, Thrasher JD, Straus DC, Madison RA, Hooper D. Detection of mycotoxins in patients with chronic fatigue syndrome. Toxins (Basel). 2013 Apr 11;5(4):605-17. doi: 10.3390/toxins5040605. PMID: 23580077; PMCID: PMC3705282.
Buckley L, MacHale SM, Cavanagh JT, Sharpe M, Deary IJ, Lawrie SM. Personality dimensions in chronic fatigue syndrome and depression. J Psychosom Res. 1999 Apr;46(4):395-400. doi: 10.1016/s0022-3999(98)00120-2. PMID: 10340240.
Chao LL, Kriger S, Buckley S, Ng P, Mueller SG. Effects of low-level sarin and cyclosarin exposure on hippocampal subfields in Gulf War Veterans. Neurotoxicology. 2014 Sep;44:263-9. doi: 10.1016/j.neuro.2014.07.003. Epub 2014 Jul 21. PMID: 25058901; PMCID: PMC5464327.
Chu, L., Valencia, I. J., Garvert, D. W., & Montoya, J. G. (2019). Onset patterns and course of myalgic encephalomyelitis/chronic fatigue syndrome. Frontiers in pediatrics, 7, 12.
Crompton, C. J., Sharp, M., Axbey, H., Fletcher-Watson, S., Flynn, E. G., & Ropar, D. (2020). Neurotype-matching, but not being autistic, influences self and observer ratings of interpersonal rapport. Frontiers in Psychology, 11, 2961.
Csecs JLL, Iodice V, Rae CL, Brooke A, Simmons R, Quadt L, Savage GK, Dowell NG, Prowse F, Themelis K, Mathias CJ, Critchley HD, Eccles JA. Joint Hypermobility Links Neurodivergence to Dysautonomia and Pain. Front Psychiatry. 2022 Feb 2;12:786916. doi: 10.3389/fpsyt.2021.786916. PMID: 35185636; PMCID: PMC8847158.
Dancey CP, Friend J. Symptoms, impairment and illness intrusiveness–their relationship with depression in women with CFS/ME. Psychol Health. 2008;23(8):983-99. doi: 10.1080/08870440701619957. PMID: 25160923.
Daniels, J., Brigden, A., & Kacorova, A. (2017). Anxiety and depression in chronic fatigue syndrome/myalgic encephalomyelitis (CFS/ME): examining the incidence of health anxiety in CFS/ME. Psychology and Psychotherapy: Theory, Research and Practice, 90(3), 502-509.
Dargenio VN, Dargenio C, Castellaneta S, De Giacomo A, Laguardia M, Schettini F, Francavilla R, Cristofori F. Intestinal Barrier Dysfunction and Microbiota-Gut-Brain Axis: Possible Implications in the Pathogenesis and Treatment of Autism Spectrum Disorder. Nutrients. 2023 Mar 27;15(7):1620. doi: 10.3390/nu15071620. PMID: 37049461; PMCID: PMC10096948.
de Magistris L, Familiari V, Pascotto A, Sapone A, Frolli A, Iardino P, Carteni M, De Rosa M, Francavilla R, Riegler G, Militerni R, Bravaccio C. Alterations of the intestinal barrier in patients with autism spectrum disorders and in their first-degree relatives. J Pediatr Gastroenterol Nutr. 2010 Oct;51(4):418-24. doi: 10.1097/MPG.0b013e3181dcc4a5. PMID: 20683204.
Dong H, Zhang X, Qian Y. Mast cells and neuroinflammation. Med Sci Monit Basic Res. 2014 Dec 21;20:200-6. doi: 10.12659/MSMBR.893093. PMID: 25529562; PMCID: PMC4282993.
Eisenlohr-Moul T, Divine M, Schmalenberger K, Murphy L, Buchert B, Wagner-Schuman M, Kania A, Raja S, Miller AB, Barone J, Ross J. Prevalence of lifetime self-injurious thoughts and behaviors in a global sample of 599 patients reporting prospectively confirmed diagnosis with premenstrual dysphoric disorder. BMC Psychiatry. 2022 Mar 19;22(1):199. doi: 10.1186/s12888-022-03851-0. PMID: 35303811; PMCID: PMC8933886.
Giloteaux, L., Goodrich, J.K., Walters, W.A. et al. Reduced diversity and altered composition of the gut microbiome in individuals with myalgic encephalomyelitis/chronic fatigue syndrome. Microbiome 4, 30 (2016).
Gotts ZM, Deary V, Newton J, Van der Dussen D, De Roy P, Ellis JG. Are there sleep-specific phenotypes in patients with chronic fatigue syndrome? A cross-sectional polysomnography analysis. BMJ Open. 2013 Jun 20;3(6):e002999. doi: 10.1136/bmjopen-2013-002999. PMID: 23794547; PMCID: PMC3669720.
Groenman AP, Torenvliet C, Radhoe TA, Agelink van Rentergem JA, Geurts HM. Menstruation and menopause in autistic adults: Periods of importance? Autism. 2022 Aug;26(6):1563-1572. doi: 10.1177/13623613211059721. Epub 2021 Nov 26. PMID: 34825585; PMCID: PMC9344571.
Engineer CT, Hays SA, Kilgard MP. Vagus nerve stimulation as a potential adjuvant to behavioral therapy for autism and other neurodevelopmental disorders. J Neurodev Disord. 2017 Jul 4;9:20. doi: 10.1186/s11689-017-9203-z. PMID: 28690686; PMCID: PMC5496407.
Espinosa P, Urra JM. Decreased Expression of the CD57 Molecule in T Lymphocytes of Patients with Chronic Fatigue Syndrome. Mol Neurobiol. 2019 Sep;56(9):6581-6585. doi: 10.1007/s12035-019-1549-7. Epub 2019 Mar 21. PMID: 30895436.
Hanahan D, Weinberg RA. Hallmarks of cancer: the next generation. Cell. 2011 Mar 4;144(5):646-74. doi: 10.1016/j.cell.2011.02.013. PMID: 21376230.
Heim C, Wagner D, Maloney E, Papanicolaou DA, Solomon L, Jones JF, Unger ER, Reeves WC. Early adverse experience and risk for chronic fatigue syndrome: results from a population-based study. Arch Gen Psychiatry. 2006 Nov;63(11):1258-66. doi: 10.1001/archpsyc.63.11.1258. PMID: 17088506.
Heim C, Nater UM, Maloney E, Boneva R, Jones JF, Reeves WC. Childhood trauma and risk for chronic fatigue syndrome: association with neuroendocrine dysfunction. Arch Gen Psychiatry. 2009 Jan;66(1):72-80. doi: 10.1001/archgenpsychiatry.2008.508. PMID: 19124690.
Kojima, M. Alexithymia as a prognostic risk factor for health problems: a brief review of epidemiological studies. BioPsychoSocial Med 6, 21 (2012). https://doi.org/10.1186/1751-0759-6-21
Kong, X., Zhu, J., Tian, R., Liu, S., Sherman, H. T., Zhang, X., … & Wan, G. (2020). Early screening and risk factors of autism spectrum disorder in a large cohort of Chinese patients with Prader-Willi syndrome. Frontiers in psychiatry, 11, 594934.
Kossewska J, Bierlit K, Trajkovski V. Personality, Anxiety, and Stress in Patients with Small Intestine Bacterial Overgrowth Syndrome. The Polish Preliminary Study. Int J Environ Res Public Health. 2022 Dec 21;20(1):93. doi: 10.3390/ijerph20010093. PMID: 36612414; PMCID: PMC9819554.
Lee M, Krishnamurthy J, Susi A, Sullivan C, Gorman GH, Hisle-Gorman E, Erdie-Lalena CR, Nylund CM. Association of Autism Spectrum Disorders and Inflammatory Bowel Disease. J Autism Dev Disord. 2018 May;48(5):1523-1529. doi: 10.1007/s10803-017-3409-5. PMID: 29170940.
Li Y, Qiu S, Shi J, Guo Y, Li Z, Cheng Y, Liu Y. Association between MTHFR C677T/A1298C and susceptibility to autism spectrum disorders: a meta-analysis. BMC Pediatr. 2020 Sep 24;20(1):449. doi: 10.1186/s12887-020-02330-3. PMID: 32972375; PMCID: PMC7517654.
Liu CH, Yang MH, Zhang GZ, Wang XX, Li B, Li M, Woelfer M, Walter M, Wang L. Neural networks and the anti-inflammatory effect of transcutaneous auricular vagus nerve stimulation in depression. J Neuroinflammation. 2020 Feb 12;17(1):54. doi: 10.1186/s12974-020-01732-5. PMID: 32050990; PMCID: PMC7017619.
Lievesley K, Rimes KA, Chalder T. A review of the predisposing, precipitating and perpetuating factors in Chronic Fatigue Syndrome in children and adolescents. Clin Psychol Rev. 2014 Apr;34(3):233-48. doi: 10.1016/j.cpr.2014.02.002. Epub 2014 Mar 1. PMID: 24632047.
Maes M, Mihaylova I, De Ruyter M. Lower serum zinc in Chronic Fatigue Syndrome (CFS): relationships to immune dysfunctions and relevance for the oxidative stress status in CFS. J Affect Disord. 2006 Feb;90(2-3):141-7. doi: 10.1016/j.jad.2005.11.002. Epub 2005 Dec 9. PMID: 16338007.
Maes M, Mihaylova I, Leunis JC. Increased serum IgA and IgM against LPS of enterobacteria in chronic fatigue syndrome (CFS): indication for the involvement of gram-negative enterobacteria in the etiology of CFS and for the presence of an increased gut-intestinal permeability. J Affect Disord. 2007 Apr;99(1-3):237-40. doi: 10.1016/j.jad.2006.08.021. Epub 2006 Sep 27. PMID: 17007934.
Maes M, Leunis JC. Normalization of leaky gut in chronic fatigue syndrome (CFS) is accompanied by a clinical improvement: effects of age, duration of illness and the translocation of LPS from gram-negative bacteria. Neuro Endocrinol Lett. 2008 Dec;29(6):902-10. PMID: 19112401.
Magnusson AE, Nias DK, White PD. Is perfectionism associated with fatigue? J Psychosom Res. 1996 Oct;41(4):377-83. doi: 10.1016/s0022-3999(96)00189-4. PMID: 8971668.
Maintz L, Novak N. Histamine and histamine intolerance. Am J Clin Nutr. 2007 May;85(5):1185-96. doi: 10.1093/ajcn/85.5.1185. PMID: 17490952.
Makris G, Agorastos A, Chrousos GP, Pervanidou P. Stress System Activation in Children and Adolescents With Autism Spectrum Disorder. Front Neurosci. 2022 Jan 13;15:756628. doi: 10.3389/fnins.2021.756628. PMID: 35095389; PMCID: PMC8793840.
Mallorquí-Bagué N, Garfinkel SN, Engels M, Eccles JA, Pailhez G, Bulbena A, Critchley HD. Neuroimaging and psychophysiological investigation of the link between anxiety, enhanced affective reactivity and interoception in people with joint hypermobility. Front Psychol. 2014 Oct 14;5:1162. doi: 10.3389/fpsyg.2014.01162. PMID: 25352818; PMCID: PMC4196473
McElhanon BO, McCracken C, Karpen S, Sharp WG. Gastrointestinal symptoms in autism spectrum disorder: a meta-analysis. Pediatrics. 2014 May;133(5):872-83. doi: 10.1542/peds.2013-3995. PMID: 24777214.
McGinnis WR, Audhya T, Walsh WJ, Jackson JA, McLaren-Howard J, Lewis A, Lauda PH, Bibus DM, Jurnak F, Lietha R, Hoffer A. Discerning the Mauve Factor, Part 1. Altern Ther Health Med. 2008 Mar-Apr;14(2):40-50. Erratum in: Altern Ther Health Med. 2008 May-Jun;14(3):15. PMID: 18383989.
McGinnis WR, Audhya T, Walsh WJ, Jackson JA, McLaren-Howard J, Lewis A, Lauda PH, Bibus DM, Jurnak F, Lietha R, Hoffer A. Discerning the Mauve factor, Part 2. Altern Ther Health Med. 2008 May-Jun;14(3):56-62. PMID: 18517107.
Monzio Compagnoni G, Di Fonzo A, Corti S, Comi GP, Bresolin N, Masliah E. The Role of Mitochondria in Neurodegenerative Diseases: the Lesson from Alzheimer’s Disease and Parkinson’s Disease. Mol Neurobiol. 2020 Jul;57(7):2959-2980. doi: 10.1007/s12035-020-01926-1. Epub 2020 May 22. PMID: 32445085; PMCID: PMC9047992.
Morris G, Berk M, Walder K, Maes M. The Putative Role of Viruses, Bacteria, and Chronic Fungal Biotoxin Exposure in the Genesis of Intractable Fatigue Accompanied by Cognitive and Physical Disability. Mol Neurobiol. 2016 May;53(4):2550-71. doi: 10.1007/s12035-015-9262-7. Epub 2015 Jun 17. PMID: 26081141.
Nakanishi G, Pita-Oliveira M, Bertagnolli LS, Torres-Loureiro S, Scudeler MM, Cirino HS, Chaves ML, Miwa B, Rodrigues-Soares F. Worldwide Systematic Review of GSTM1 and GSTT1 Null Genotypes by Continent, Ethnicity, and Therapeutic Area. OMICS. 2022 Oct;26(10):528-541. doi: 10.1089/omi.2022.0090. Epub 2022 Sep 16. PMID: 36112350.
Peters SL, Yao CK, Philpott H, Yelland GW, Muir JG, Gibson PR. Randomised clinical trial: the efficacy of gut-directed hypnotherapy is similar to that of the low FODMAP diet for the treatment of irritable bowel syndrome. Aliment Pharmacol Ther. 2016 Sep;44(5):447-59. doi: 10.1111/apt.13706. Epub 2016 Jul 11. PMID: 27397586.
Poznyak AV, Ivanova EA, Sobenin IA, Yet SF, Orekhov AN. The Role of Mitochondria in Cardiovascular Diseases. Biology (Basel). 2020 Jun 25;9(6):137. doi: 10.3390/biology9060137. PMID: 32630516; PMCID: PMC7344641.
Rasa S, Nora-Krukle Z, Henning N, Eliassen E, Shikova E, Harrer T, Scheibenbogen C, Murovska M, Prusty BK; European Network on ME/CFS (EUROMENE). Chronic viral infections in myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS). J Transl Med. 2018 Oct 1;16(1):268. doi: 10.1186/s12967-018-1644-y. PMID: 30285773; PMCID: PMC6167797.
Rauch SAM, King A, Kim HM, Powell C, Rajaram N, Venners M, Simon NM, Hamner M, Liberzon I. Cortisol awakening response in PTSD treatment: Predictor or mechanism of change. Psychoneuroendocrinology. 2020 Aug;118:104714. doi: 10.1016/j.psyneuen.2020.104714. Epub 2020 May 15. PMID: 32446108; PMCID: PMC7984524.
Reynolds, A. M., Soke, G. N., Sabourin, K. R., Hepburn, S., Katz, T., Wiggins, L. D., Schieve, L. A., & Levy, S. E. (2019). Sleep Problems in 2- to 5-Year-Olds With Autism Spectrum Disorder and Other Developmental Delays. Pediatrics, 143(3), e20180492. https://doi.org/10.1542/peds.2018-0492
Sandin S, Lichtenstein P, Kuja-Halkola R, Hultman C, Larsson H, Reichenberg A. The Heritability of Autism Spectrum Disorder. JAMA. 2017 Sep 26;318(12):1182-1184. doi: 10.1001/jama.2017.12141. PMID: 28973605; PMCID: PMC5818813.
Sharp HEC, Critchley HD, Eccles JA. Connecting brain and body: Transdiagnostic relevance of connective tissue variants to neuropsychiatric symptom expression. World J Psychiatry. 2021 Oct 19;11(10):805-820. doi: 10.5498/wjp.v11.i10.805. PMID: 34733643; PMCID: PMC8546774.
Schmidt R, Hiemisch A, Kiess W, von Klitzing K, Schlensog-Schuster F, Hilbert A. Macro- and Micronutrient Intake in Children with Avoidant/Restrictive Food Intake Disorder. Nutrients. 2021 Jan 27;13(2):400. doi: 10.3390/nu13020400. PMID: 33513954; PMCID: PMC7911718.
Shoemaker RC, House D, Ryan JC. Structural brain abnormalities in patients with inflammatory illness acquired following exposure to water-damaged buildings: a volumetric MRI study using NeuroQuant®. Neurotoxicol Teratol. 2014 Sep-Oct;45:18-26. doi: 10.1016/j.ntt.2014.06.004. Epub 2014 Jun 17. PMID: 24946038.
Sotzny F, Blanco J, Capelli E, Castro-Marrero J, Steiner S, Murovska M, Scheibenbogen C; European Network on ME/CFS (EUROMENE). Myalgic Encephalomyelitis/Chronic Fatigue Syndrome – Evidence for an autoimmune disease. Autoimmun Rev. 2018 Jun;17(6):601-609. doi: 10.1016/ j.autrev.2018.01.009. Epub 2018 Apr 7. PMID: 29635081.
Springer A, Oleksa-Marewska K, Basińska-Zych A, Werner I, Białowąs S. Occupational burnout and chronic fatigue in the work of academic teachers-moderating role of selected health behaviours. PLoS One. 2023 Jan 26;18(1):e0280080. doi: 10.1371/journal.pone.0280080. PMID: 36701360; PMCID: PMC9879519.
Szyf M. The epigenetics of early life adversity and trauma inheritance: an interview with Moshe Szyf. Epigenomics. 2022 Mar;14(6):309-314. doi: 10.2217/epi-2021-0483. Epub 2021 Dec 8. PMID: 34877868.
Theoharides TC, Kavalioti M, Tsilioni I. Mast Cells, Stress, Fear and Autism Spectrum Disorder. Int J Mol Sci. 2019 Jul 24;20(15):3611. doi: 10.3390/ijms20153611. PMID: 31344805; PMCID: PMC6696098.
Tomas C, Newton J, Watson S. A review of hypothalamic-pituitary-adrenal axis function in chronic fatigue syndrome. ISRN Neurosci. 2013 Sep 30;2013:784520. doi: 10.1155/2013/784520. PMID: 24959566; PMCID: PMC4045534.
Traianos E, Dibnah B, Lendrem D, et alAB0051 THE EFFECTS OF NON-INVASIVE VAGUS NERVE STIMULATION ON IMMUNOLOGICAL RESPONSES AND PATIENT REPORTED OUTCOME MEASURES OF FATIGUE IN PATIENTS WITH CHRONIC FATIGUE SYNDROME, FIBROMYALGIA, AND RHEUMATOID ARTHRITISAnnals of the Rheumatic Diseases 2021;80:1057-1058.
Tsai SY, Chen HJ, Lio CF, Kuo CF, Kao AC, Wang WS, Yao WC, Chen C, Yang TY. Increased risk of chronic fatigue syndrome in patients with inflammatory bowel disease: a population-based retrospective cohort study. J Transl Med. 2019 Feb 22;17(1):55. doi: 10.1186/s12967-019-1797-3. PMID: 30795765; PMCID: PMC6387539.
Tsilioni I, Patel AB, Pantazopoulos H, Berretta S, Conti P, Leeman SE, Theoharides TC. IL-37 is increased in brains of children with autism spectrum disorder and inhibits human microglia stimulated by neurotensin. Proc Natl Acad Sci U S A. 2019 Oct 22;116(43):21659-21665. doi: 10.1073/pnas.1906817116. Epub 2019 Oct 7. PMID: 31591201; PMCID: PMC6815178.
van Rensburg R, Meyer HP, Hitchcock SA, Schuler CE. Screening for Adult ADHD in Patients with Fibromyalgia Syndrome. Pain Med. 2018 Sep 1;19(9):1825-1831. doi: 10.1093/pm/pnx275. PMID: 29099955.
Wang SX, Wu WC. Effects of psychological stress on small intestinal motility and bacteria and mucosa in mice. World J Gastroenterol. 2005 Apr 7;11(13):2016-21. doi: 10.3748/wjg.v11.i13.2016. PMID: 15800998; PMCID: PMC4305729.
Wang T, Yin J, Miller AH, Xiao C. A systematic review of the association between fatigue and genetic polymorphisms. Brain Behav Immun. 2017 May;62:230-244. doi: 10.1016/j.bbi.2017.01.007. Epub 2017 Jan 12. PMID: 28089639; PMCID: PMC5947855.
Weiss RB, Stange JP, Boland EM, Black SK, LaBelle DR, Abramson LY, Alloy LB. Kindling of life stress in bipolar disorder: comparison of sensitization and autonomy models. J Abnorm Psychol. 2015 Feb;124(1):4-16. doi: 10.1037/abn0000014. PMID: 25688428; PMCID: PMC4332547.
Wojcik DP, Godfrey ME, Christie D, Haley BE. Mercury toxicity presenting as chronic fatigue, memory impairment and depression: diagnosis, treatment, susceptibility, and outcomes in a New Zealand general practice setting (1994-2006). Neuro Endocrinol Lett. 2006 Aug;27(4):415-23. PMID: 16891999.
Yang EV, Webster Marketon JI, Chen M, Lo KW, Kim SJ, Glaser R. Glucocorticoids activate Epstein Barr virus lytic replication through the upregulation of immediate early BZLF1 gene expression. Brain Behav Immun. 2010 Oct;24(7):1089-96. doi: 10.1016/j.bbi.2010.04.013. Epub 2010 May 11. PMID: 20466055; PMCID: PMC2939213.
Yap CX, Henders AK, Alvares GA, Wood DLA, Krause L, Tyson GW, Restuadi R, Wallace L, McLaren T, Hansell NK, Cleary D, Grove R, Hafekost C, Harun A, Holdsworth H, Jellett R, Khan F, Lawson LP, Leslie J, Frenk ML, Masi A, Mathew NE, Muniandy M, Nothard M, Miller JL, Nunn L, Holtmann G, Strike LT, de Zubicaray GI, Thompson PM, McMahon KL, Wright MJ, Visscher PM, Dawson PA, Dissanayake C, Eapen V, Heussler HS, McRae AF, Whitehouse AJO, Wray NR, Gratten J. Autism-related dietary preferences mediate autism-gut microbiome associations. Cell. 2021 Nov 24;184(24):5916-5931.e17. doi: 10.1016/j.cell.2021.10.015. Epub 2021 Nov 11. PMID: 34767757.
Yuzefovych LV, Pastukh VM, Ruchko MV, Simmons JD, Richards WO, Rachek LI. Plasma mitochondrial DNA is elevated in obese type 2 diabetes mellitus patients and correlates positively with insulin resistance. PLoS One. 2019 Oct 10;14(10):e0222278. doi: 10.1371/journal.pone.0222278. PMID: 31600210; PMCID: PMC6786592.