Diagnostic and Statistical Manual of Mental Disorders (DSM-5) in Pictures
I am back with week 4 of my DSM-5 in pictures series (you can check out autism here, and ADHD here).
Disclaimers, FAQs, & Basic Information on the DSM-5
Why am I creating this series: I am creating this series to increase the accessibility and transparency of the DSM-5 and the clinical tools people like me use when we are giving you (or anyone) a diagnosis. I find the mental health world can be overly mysterious, increasing anxiety and stress for many. I believe this process should be as understandable and transparent as possible. I am using visuals to break down the DSM-5 because, like many neurodivergent people, unless a thing is visual, I have a hard time understanding it!
Disclaimers: This is for educational purposes only and isn’t intended as a substitute for medical advice or to be used as a primary diagnostic tool.
A word on language: I use direct language from the DSM. This is for educational purposes. Much of the language used is deficit-based and pathological in nature. It doesn’t mean I agree with all the wording (in fact, I do not!). I have made this choice to increase the transparency of what is actually in the DSM.
What about international people? The Diagnostic and Statistical Manual is based in the United States (the American Psychiatric Association puts it out). However, the criteria are very similar to the ICD, which is used globally and broadly in medical settings.
Okay, now that we’ve gone over the purpose, intent, and limits of this post. Let’s dive in!
What is Borderline Personality Disorder?

Borderline Personality Disorder (BPD) is a personality disorder characterized by a pervasive pattern of instability. More specifically, Borderline Personality Disorder is characterized by instability in relationships, self-image, emotions, and behavior (impulsivity).
Borderline Personality Disorder has a prevalence rate of 5.9% and is diagnosed in females at higher rates.
Borderline Personality Disorder is characterized by:
Intense difficulties in interpersonal relationships
An unstable self-concept
Impulsivity, disinhibition, and risk-taking behaviors
Difficulty managing painful emotions
To receive a diagnosis of Borderline Personality Disorder, these symptoms must:
1) Be present in multiple contexts (home and school or home and work)
2) Result in significant suffering or cause significant impairment in functioning
What Causes Borderline Personality Disorder
While no specific “cause” has been identified, several risk factors for BPD have been identified. Dominant theories of BPD suggest that it results when a person who has an innate vulnerability (genetics) interacts with a “chronically invalidating environment” (Vanwoerden et al., 2019).
The DSM-5 Criteria for Borderline Personality Disorder
To meet the criteria for Borderline Personality Disorder, five of nine symptoms must be present. They must be present in multiple contexts and cause significant suffering or impairment in relationships and overall functioning. The nine criteria of Borderline Personality Disorder include:

1. Frantic efforts to avoid real or imagined abandonment.
2. A pattern of unstable and intense interpersonal relationships characterized by alternating between extremes of idealization and devaluation.
3. Identity disturbance: markedly and persistently unstable self-image or sense of self.
4. Impulsivity in at least two potentially self-damaging areas (e.g., spending, sex, substance abuse, reckless driving, binge eating).
5. Recurrent suicidal behavior, gestures or threats, or self-mutilating behavior.
6. Affective instability due to a marked reactivity of mood (e.g., intense episodic dysphoria, irritability, or anxiety usually lasting a few hours and rarely more than a few days).
7. Chronic feelings of emptiness.
8. Inappropriate, intense anger or difficulty controlling anger (e.g., frequent displays of temper, constant anger, recurrent physical fights).
9. Transient, stress-related paranoid ideation or severe dissociative symptoms.
A Brief Conceptualization of Borderline Personality Disorder
Before reviewing the symptoms of BPD in more detail, I want to provide context for why these symptoms make sense. BPD is a heavily stigmatized condition. When we just talk about symptoms and don’t consider why these symptoms make sense, we perpetuate the stigma associated with BPD.
At the core of BPD is a very anxious-preoccupied attachment style (in the context of BPD, this is typically a trauma response to early attachment injury). People with this attachment structure tend to believe “I am bad, and others are good.” As such, they often feel insecure and anxious in their relationships. They have a strong need to belong, fit in, and feel accepted. When an attachment (relationship) goes awry (or is perceived to go awry), this tends to confirm to the person that they are worthless and bad. A breakdown in a relationship can cause an intense pain/shame/anger response.
A person with an anxious-preoccupied attachment structure cannot be okay when the relationship is not okay. When there is tension or distance in the relationship, the person struggles to self-soothe (fixing the relationship is what soothes them). This can lead to frantic efforts to repair the relationship or to protest the rupture (lashing out). This can overwhelm the other person leading to further attachment withdrawal.
A person with an anxious attachment style is also primed to look for attachment ruptures. Their minds are constantly scanning the environment looking for signals of rejection. When our minds do this, we tend to over-interpret events as signs of rejection, which can cause the person to interpret something neutral as a sign of rejection. This is the brain’s attempt to be on hyper-alert—it is trying to protect the person by being hyper-aware of signs of rejection. Ultimately, it ends up causing the person more suffering.
Attachment injury invokes such intense feelings of shame, badness, and rejection that it tends to overwhelm the person. These feelings are so intense and painful to metabolize that they can often be turned outward to the world through a process known as projection.
When some emotions are excruciating, we tend to push them away by projecting them onto others. In projection, we act in a way that causes the other person to feel what we are too afraid to feel. For example, when a child feels powerless, they may have a significant tantrum and won’t respond to redirection, causing the parent to feel powerless. The child doesn’t have words for this, but through an unconscious process, they invite their parent to metabolize the emotions too big for them to metabolize.
In the case of BPD, the experience of being rejected is an emotion often too overwhelming to metabolize. The person may therefore project this onto the other by making the other person feel rejected (through belittling, angry outbursts, or more). This is not a conscious process and often feels outside the person’s control. However, learning DBT skills and healing attachment wounds can lead to much more conscious action and agency.
Now that we have some context for why these symptoms make sense let’s now turn to the specific symptom of Borderline Personality Disorder.
Criteria One: Intense Fear of Abandonment
People with BPD often experience an intense fear of abandonment. This can result in frantic efforts to avoid real or imagined abandonment.
Common triggers include:
Upcoming separation
Rejection (or even the perception of rejection)
Perception of being neglected
A loss of external structure
These situations can result in profound changes in a person’s self-image, emotional stability, thoughts, and behavior. This hyper-sensitivity to relational shifts can result in strong reactions, often involving inappropriate anger. The person’s responses will seem disproportional to the situation.
Separation situations that are planned or unavoidable will still create a strong sense of despair for the person and may result in extreme protest behavior and actions. The perceived abandonment often reinforces the belief that the person is “bad” and invokes their general fear of being alone.
Criteria Two: Unstable Relationships

People with Borderline Personality Disorder often experience instability in interpersonal relationships. Interpersonal challenges are often characterized by unstable and intense relationships that shift between idealization and devaluation. There is often a marked interpersonal sensitivity with extreme efforts (often interpreted as manipulation) to avoid abandonment (Weiner et al. 2019).
A person with Borderline Personality Disorder often idealizes potential partners, lovers, and caregivers early in the relationship. This can result in quick and fast bonds (spending lots of time together and sharing intimate details quickly in the relationship).
The relationship can shift quickly (particularly if there is perceived rejection or abandonment). They may feel (and accuse) the other person of not genuinely caring or not being there for them.
There are often sudden and dramatic shifts in relationships. Someone who was once perceived as caring, kind, and wonderful can be seen as cruel and punitive the next moment.
This shift often takes place when the idealized image breaks down. One way of thinking about this dynamic is as despair turned outward. The despair is too painful to metabolize, so it is turned outward through devaluation and anger.
Criteria Three: Unstable Self-Image
A person with BPD often experiences a diffuse sense of self that is prone to sudden and dramatic shifts of identity.
These changes are often characterized by
shifting goals and future plans
sexual and gender identities
values
political ideologies
views on friendships
career decisions
One extreme form is when the person changes from the role of being a “needy supplicant” to that of a “righteous avenger of past mistreatment” (DSM-5). This can result in false accusations of previous caregivers and partners. (Note: for the person, it won’t feel like they are making a false accusation, as the accusation aligns with their perceived experience of what happened.)
At other times this instability may show up as a general sense of not existing. These experiences typically occur when the person feels a lack of connection and of meaningful, nurturing, and supportive relationships. Due to the need for structure and meaning, people with BPD typically do best with structured work and school environments.
Criteria Four: Impulsivity (Self-Damaging)
People with Borderline Personality Disorder often “display impulsivity in at least two areas that are potentially self-damaging.”

This may include:
- gambling
- spending money irresponsibly
- binge eating
- abusing substances
- engaging in unsafe sex
- reckless driving.
ADHD vs. Borderline PersonalityDisorder
$10.00
Self-damaging impulsivity typically occurs in response to perceived rejection or abandonment and is typically a response to emotional dysregulation.
(Note: while this may look similar to ADHD impulsivity, it is distinct from it and has different causes. To learn more about the similarities and differences between ADHD and BPD, check out the ebook here).
Criteria Five: Recurrent Suicidal Behavior & Self-Harm

People with Borderline Personality disorder often experience recurrent suicidal behavior, gestures, suicidal threats, or self-harming behavior.
These behaviors are often triggered by fear of abandonment and abandonment reactions. These behaviors can also be a response to emotional dysregulation and dissociative experience.
While the prevalence rates of self-harm have been estimated to be around 17% in adolescents and 6% in adult samples of the general population, the prevalence rates among people with BPD are 95% (adolescents) and 90% (adults) (Reichl & Kaess, 2021).
Self-harm can function to serve several purposes (it may be a reaction to emotional dysregulation or dissociative experiences). Self-harm in BPD is most often related to attachment injury and relationship conflict (Dudas, 2017).
While there are many reasons a person engages in self-harm, the most common reason among people with BPD is related to emotional regulation. Over 95% of women with BPD identified engaging in self-harm for emotional relief (Colle et al., 2020).
Criteria Six: Affective Instability
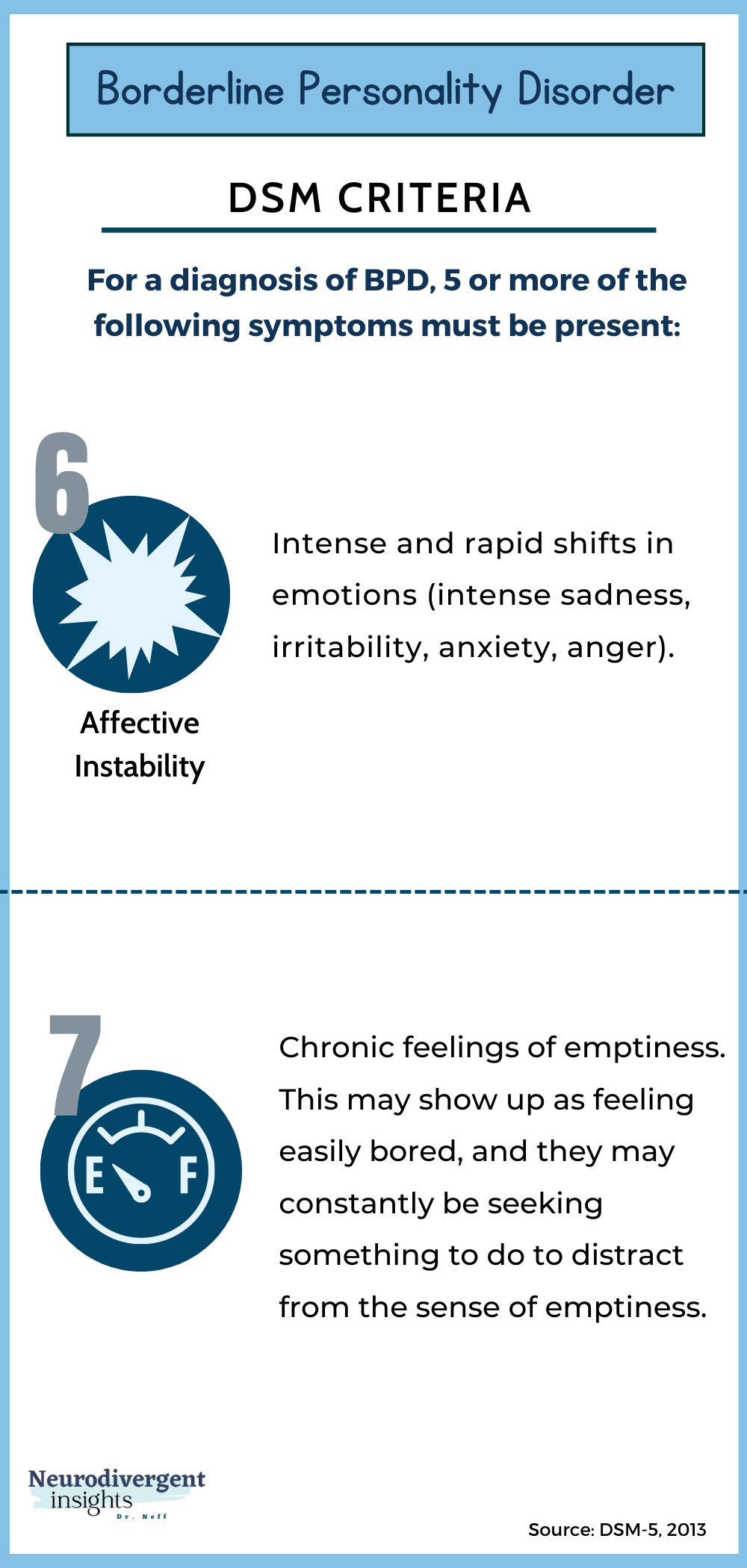
People with BPD tend to experience intense and rapid shifts in emotions. They often experience heightened emotional sensitivity. Something that may seem small to someone else can result in big emotions (intense sadness, irritability, anxiety, anger).
People with Borderline Personality Disorder are more likely to experience emotional stress and affective instability related to perceived abandonment and relationship stress. Relationship tension can lead to a sense of hopelessness and frantic panic (Littman, E., 2021).
The person’s baseline mood tends to be “dysphoric” (sad, depressed), with limited access to the positive emotions of joy, happiness, and hope. The person’s baseline depressed mood is often disrupted by periods of anger, panic, or despair.
Criteria Seven: Chronic Feelings of Emptiness

People with Borderline Personality Disorder are often plagued with chronic feelings of emptiness.
This may show up as feeling easily bored, and they may constantly be seeking something to do to distract from the sense of emptiness.
(*Note this can look similar to the ADHD need for stimulation and difficulty with resting or similar to a diffuse sense of self often seen in high-masking Autism). To read more about the similarities and differences between Autism and BPD, you can read about it in my ebook here.
Criteria Eight: Inappropriate Anger

People with BPD often experience difficulty controlling their anger which can manifest as intense forms of angry outbursts. This may present as belittling others through extreme sarcasm or verbal outbursts, and it can also present as persistent bitterness directed at others.
Anger is often triggered when a caregiver, partner, or intimate friend is perceived as being neglectful, withholding, or abandoning. Such expressions of anger are often followed by shame and guilt, leading to a negative and shame-based view of self.
Criteria Nine: Paranoid Ideation & Dissociation
Borderline Personality Disorder, ADHD, and Autism

And since this website is primarily about autism and ADHD. Before concluding this article, here are a few considerations about Borderline Personality Disorder, ADHD, and Autism.
Co-Occurring BPD, ADHD, and Autism
BPD co-occurs with ADHD & Autism at higher rates (than seen in the non-ADHD & Autistic population). In fact, the prevalence rate of nearly all Personality Disorders is higher among the ADHD & Autistic neurotype.
Our neurotype makes us more vulnerable to developing PTSD after acute trauma. It also makes us more vulnerable to developing Personality Disorders. This makes sense. We have more vulnerable nervous systems, sensory systems & amygdalas, so our bodies respond more intensely to trauma. We also experience more victimization, discrimination, & ableism. To have an innate neurodivergence is to live with many extra vulnerabilities that predispose us to things like PTSD and Personality Disorders.
Misdiagnosis
Outside of co-occurrence, BPD is also a common misdiagnosis of Autistic & ADHD people (particularly women & genderqueer people). To an untrained eye, several ADHD traits (impulsivity, hyperactivity, difficulty regulating emotions) can look like BPD.
To the untrained eye, common experiences for the high-masking Autistic can look like BPD (a diffuse sense of self from masking, sensory overload can look like angry outbursts, & difficulty with emotions & relationships).
For this reason, whenever a person is being assessed for BPD, I think it is critically important that Autism and ADHD also be considered (as either occurring alongside the BPD or instead of the BPD). If you want to learn more about the overlapping occurrences, traits, and more, you can check out my Misdiagnosis Ebook series, where I go into more detail on these topics.