Obsessive-Compulsive Disorder (OCD) is notably more prevalent among individuals who are Autistic or have ADHD. The presence of OCD can intertwine intricately with these neurodivergent experiences, sometimes making it challenging to discern whether behaviors are manifestations of Autism, ADHD, or OCD itself. Reflecting on my own childhood, I vividly recall a specific goodbye ritual with my parents. Each morning, it was imperative for me to say, ‘Goodbye, I love you, don’t die.’ Forgetting these words would plunge me into a whirlpool of anxiety that lasted until I could return home and ensure their safety. Back then, it might have seemed like just an Autistic quirk or a peculiar ritual. But now, with a deeper understanding, I recognize it as a manifestation of OCD.
As we delve deeper into this article, we’ll explore why these rituals were indicative of OCD and not solely Autistic behaviors.
It is not rare for Obsessive-Compulsive Disorder to intersect with autism or ADHD, adding a layer to the already complex tapestry of neurodivergence. Distinguishing between OCD, Autism, and ADHD isn’t just an academic exercise. It’s a vital step in providing the right support for each individual. In this discussion, we aim to broaden your understanding of how OCD interacts within the realm of neurodivergence, specifically focusing on:
The intersection of OCD and Neurodivergence
The co-occurrence of ADHD and OCD
The co-occurrence of Autism and OCD
Exploring the difference between compulsions, ADHD compensatory strategies and Autistic rituals
Understanding Obsessive-Compulsive Disorder
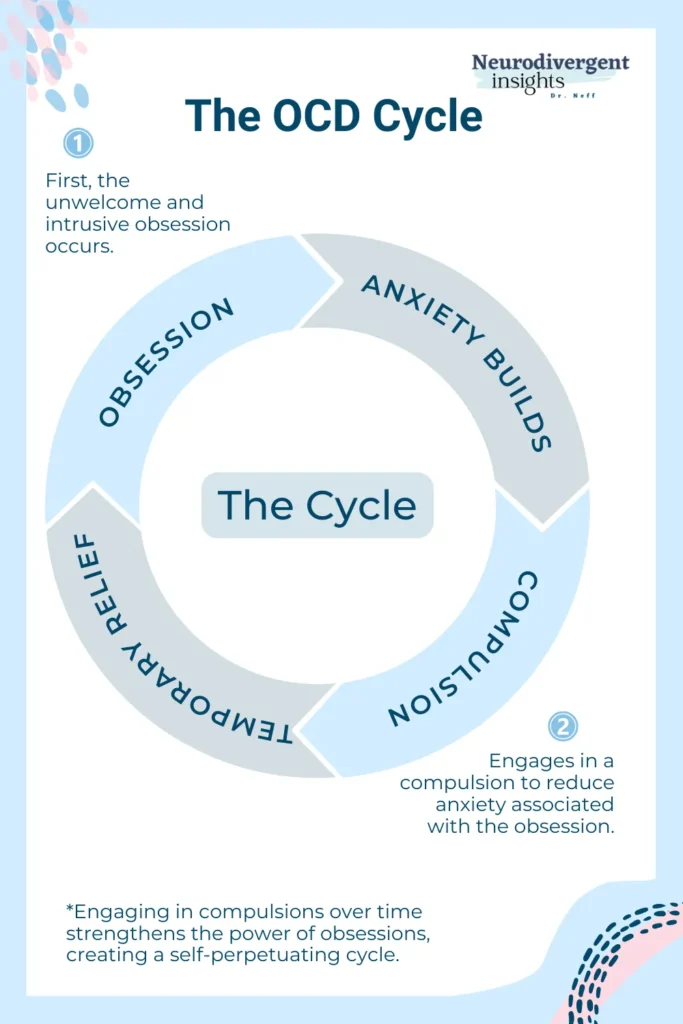
Obsessive-Compulsive Disorder, or OCD, is marked by persistent, distressing thoughts, urges, or images (obsessions) and repetitive actions (compulsions). The compulsions function to try to reduce the anxiety from the obsessions. For instance, someone might fear germs excessively, leading to constant hand-washing. These compulsions might offer temporary relief but actually increase anxiety and obsessions in the long run. Treatment usually involves therapy, like exposure and response prevention (ERP), and sometimes medication.
Is OCD a Form of Neurodivergence?
Absolutely, OCD is indeed a form of neurodivergence. Neurodivergence refers to the diversity of the human brain and cognition, encompassing a range of conditions and neurotypes like Autism, ADHD, Dyslexia, traumatic brain injury, PTSD, and, indeed, OCD. These conditions represent natural variations in the human brain.
OCD occupies a unique space within the spectrum of neurodivergence, presenting a more complex classification compared to Autism or ADHD. My journey as an Autistic-ADHD is lifelong and integral to who I am. However, my experience with OCD feels different. While I may always possess a brain prone to obsessive tendencies, OCD itself can ebb and flow, responding to treatment in ways that can significantly alter its impact on my life. It’s this responsive nature of OCD that brings into question whether it should be classified strictly as a neurotype or perhaps as a form of situational neurodivergence. There’s a nuanced debate here: Is OCD a permanent fixture of one’s neurological wiring, or is it more of a condition that can be managed or altered over time? *
How we define our relationship with OCD is deeply personal and varies widely. While I describe my experience as ‘having OCD,’ viewing it as a condition I manage and treat, others may perceive OCD as an integral part of their neurotype, shaping their identity and interactions with the world. This variety in how we view and relate to OCD underscores the condition’s multifaceted nature and our unique, individual journeys with it. What matters most is finding a way to frame our experience with OCD that feels authentic to us, empowering our approach to challenges with understanding, gentleness, and hope. There is no one-size-fits-all way to perceive or discuss OCD, and embracing this diversity of perspectives is key to a deeper, more empathy.
You can read more about the nuances of OCD here. But for now, let’s shift to exploring the co-occurrence of OCD and ADHD and OCD and autism.
Co-occurrence of OCD with ADHD and Autism
Complicating matters, OCD frequently co-occurs with innate forms of neurodivergence like ADHD and Autism! When this occurs, it can complicate both the OCD and the ADHD or Autism and create treatment complications all around! First, let’s take a closer look at OCD and ADHD, and then we’ll explore OCD and autism.
Exploring the Overlap of OCD and ADHD
In my journey both as a psychologist and as a member of the neurodivergent community, I’ve seen firsthand how the co-occurrence of Obsessive-Compulsive Disorder (OCD) and Attention-Deficit/Hyperactivity Disorder (ADHD) is not uncommon. It’s a conjunction that I’ve frequently encountered in my professional practice and within the broader neurodivergent community. Research echoes this observation, indicating that a notable number of individuals with ADHD also experience symptoms of OCD and vice versa.
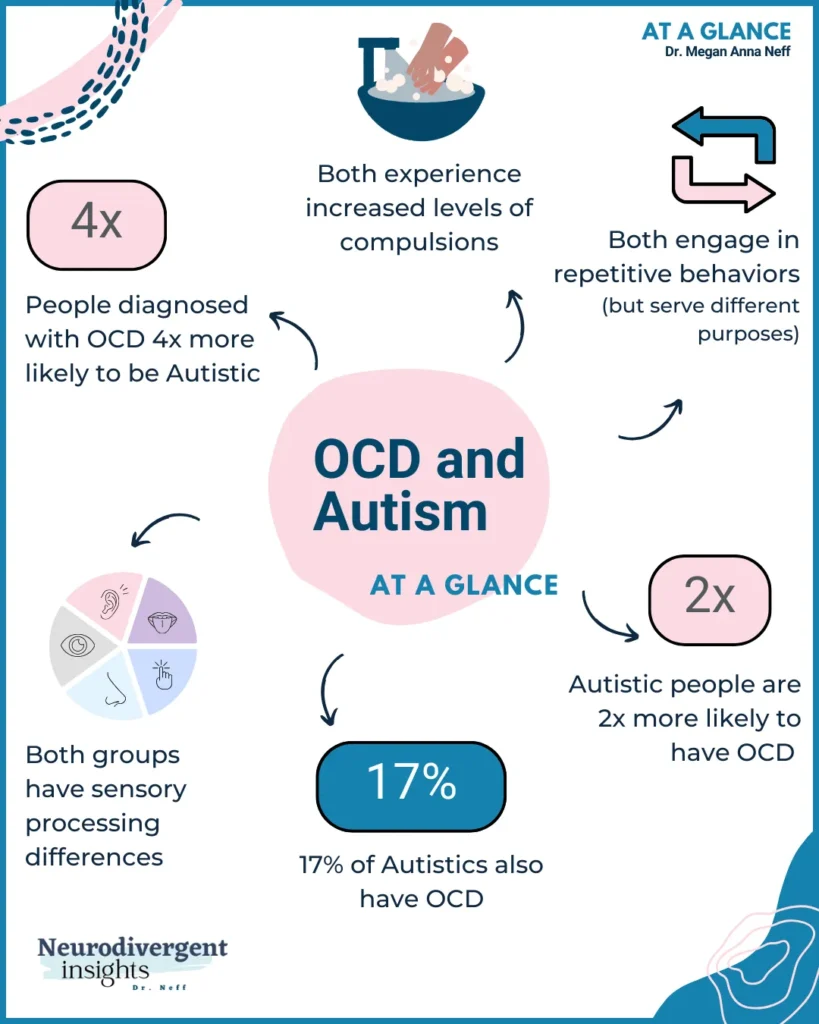
The prevalence varies, with some studies suggesting that up to 30% of individuals with OCD may also have ADHD, while others report a lower range of around 8% (Brem et al., 2014). Similarly, the presence of OCD symptoms in those with ADHD ranges between 17-25% (Masi, 2010). ADHD is the most common co-occurring condition among early-onset OCD (Brem et al., 2014).
The reasons behind this overlap aren’t entirely clear. However, there’s a growing understanding that shared genetic and neurobiological factors might be at play. Both OCD and ADHD involve challenges in executive functioning and cognitive control, which might contribute to their co-occurrence. It’s like having a mind that’s constantly juggling between the intense focus of OCD and the scattered attention of ADHD, creating a unique set of challenges.
When an individual navigates life with both OCD and ADHD, it presents a complex puzzle for diagnosis and treatment. The presence of ADHD can complicate how OCD symptoms manifest and respond to treatment. Conversely, OCD can intensify the difficulties in cognitive control and attention associated with ADHD as executive function becomes more crowded out with intrusive obsessions, which intensify focus and inattention struggles.
Chasing Thoughts and Swatting Obsessions
My son and I co-created many metaphors when he was navigating the thick of his OCD. One co-created metaphor that powerfully encapsulates his experience living with both ADHD and OCD included a beehive.
He likened his brain to a beehive, bustling with activity. In this metaphor, the hive’s numerous holes represent the myriad ideas escaping his mind, which he associated with his ADHD. Meanwhile, the bees – symbolizing his OCD obsessions – demanded relentless attention. This left him in a constant state of vigilance, trying to fend off these ‘bees’ while also attempting to manage the flow of thoughts slipping through the ‘holes.’
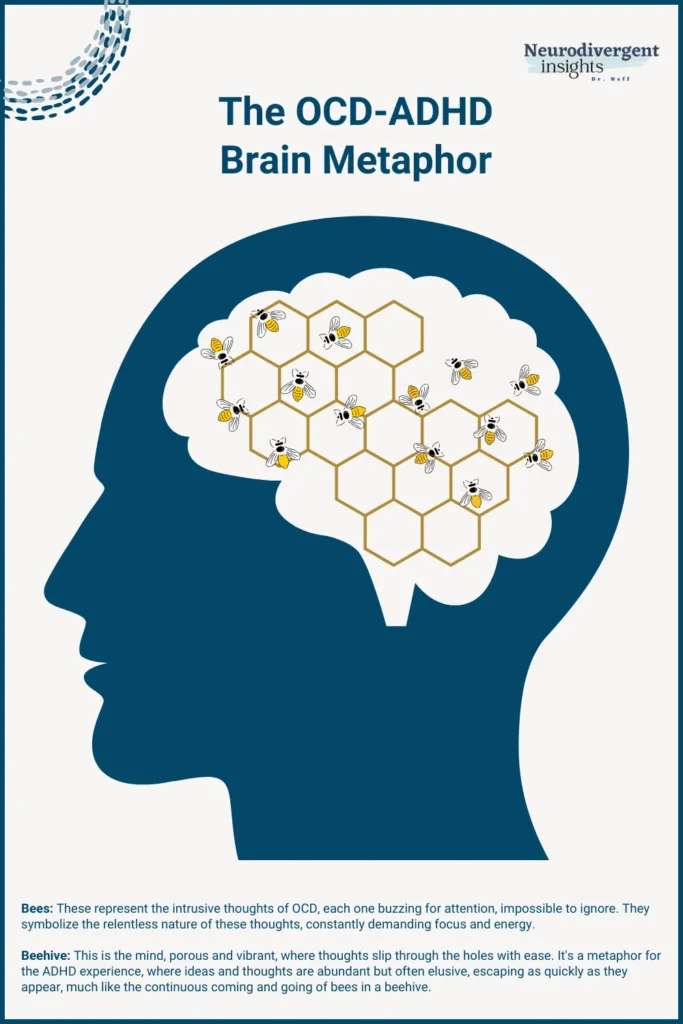
During the most intense periods of his OCD, this dynamic became overwhelming. His ability to focus on schoolwork dwindled significantly. The intrusive nature of his OCD obsessions, layered atop his ADHD, created a particularly complex and challenging situation. It’s a powerful illustration of how these conditions can intertwine, each amplifying the other, and profoundly impacting daily life.
When someone journeys through life with both OCD and ADHD, they’re navigating a complex puzzle that affects every aspect of their daily living. ADHD can color the way OCD manifests, perhaps making traditional treatments less straightforward. Conversely, OCD can add layers to the ADHD experience, intensifying struggles with focus and attention. It’s like walking a tightrope between two worlds, each with its own set of rules and challenges.
Exploring the Overlap of OCD and Autism
The intertwining paths of Obsessive-Compulsive Disorder (OCD) and autism also hold both personal and professional significance for me. It’s a connection more common than many might expect. Research indicates that a significant number of Autistic people – possibly up to 37% – also navigate the challenges of OCD.
The way OCD manifests in Autistic individuals varies greatly, necessitating a careful and thoughtful approach to both diagnosis and treatment. It’s about seeing beyond the clinical symptoms to see the internal experience behind them, to understand the person’s world and how these conditions intersect in their life.
For individuals and families living at this crossroads of OCD and autism, the journey is filled with some unique challenges. It impacts daily life profoundly, influencing overall well-being. For example, OCD may amplify sensory struggles, changes to routines, or social stress. Autistic processing may complicate OCD treatment (spoiler: we do best when treatment is adapted for our Autistic brains), and exposures may involve more stress on our already stressed systems, requiring more patience and persistence.
Recognizing this, it becomes essential to offer support that is not just comprehensive but also deeply attuned to our specific sensory needs and brain style.
Teasing Apart ADHD, Autism, and OCD
When it comes to distinguishing between ADHD, Autism, and OCD, teasing apart these conditions can be challenging. It is always advisable to collaborate with a knowledgeable clinician who comprehends the nuances of these neurodivergences and can conduct a comprehensive evaluation. Personally, I find that one key aspect to consider while differentiating these conditions is the role of OCD compulsions. To gain a deeper insight, we must delve into an individual’s subjective and internal experiences to fully grasp the significance of their outward behaviors. So, let’s briefly explore compulsions and how they can illuminate the distinctions between these neurodivergent experiences.
What is an OCD Compulsion?
At the core of Obsessive-Compulsive Disorder (OCD) lie compulsions – those often irresistible urges compelling individuals to engage in specific behaviors or actions. Imagine being driven by an internal force that relentlessly insists these actions, no matter how repetitive or time-consuming they may be, are absolutely necessary to avert something dreadful from occurring. This is the daily reality experienced by many people with OCD.
A compulsion serves as a temporary solution to alleviate the unrelenting pressure of an obsession. For instance, if someone grapples with a profound fear of contamination, their compulsion might manifest as an obsessive handwashing ritual. This action, albeit temporarily, ‘neutralizes’ the distress stemming from the obsession. It provides a fleeting respite within an ongoing cycle of anxiety and momentary relief. As illustrated in the introductory paragraph, the phrase “goodbye, love you, don’t die” to my parents served as a compulsion aimed at warding off a tragic event.
Compulsions can manifest in both overt and covert forms. Overt compulsions involve visible rituals such as handwashing, checking, or meticulously arranging objects. On the other hand, covert compulsions are internal and less conspicuous. They may encompass mental rituals like silently repeating phrases, counting, praying or reviewing memories. The concealed nature of these internal compulsions can render OCD more challenging to recognize and comprehend, both for the individuals affected and those in their immediate circles.
Examples of Compulsions in OCD:
Checking and Rechecking: Repeatedly verifying if doors are locked or appliances are turned off.
Counting: Feeling compelled to count objects or perform actions a specific number of times.
Handwashing: Excessive cleaning and handwashing, driven by fears of contamination.
Arranging and Ordering: Needing things to be in a specific order or symmetry.
Repeating Words or Phrases: Silently or aloud, often to counteract negative thoughts or fears.
Mental Rituals: Performing mental actions, like praying or thinking ‘good’ thoughts to neutralize ‘bad’ thoughts.
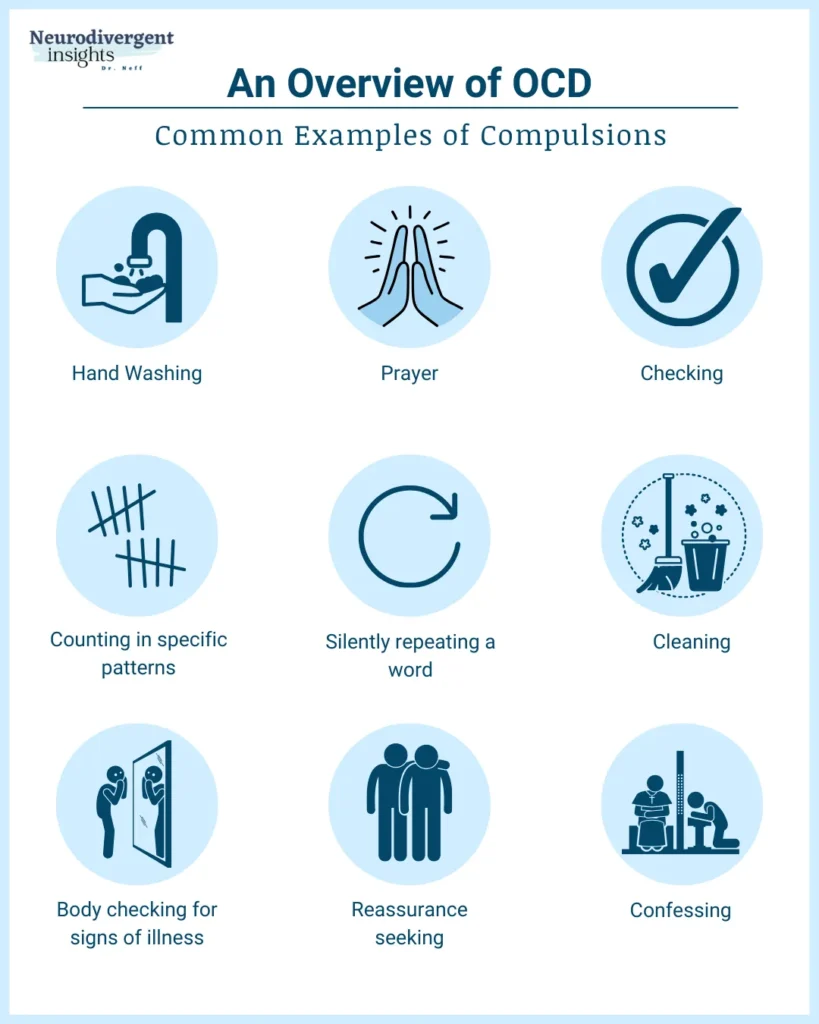
Compulsions, whether external or internal, significantly impact a person’s daily life and functioning. They are more than just habits or quirks; they are intense responses to deeply rooted anxieties.
How to tease apart compulsions from Autistic rituals
Understanding the difference between compulsions in OCD and rituals in autism is tricky but crucial, as they stem from different roots and serve distinct purposes.
Compulsions in OCD:
Compulsions are driven by a need to reduce the intense anxiety stemming from obsessive thoughts, urges, or images. Engaging in a compulsion may offer momentary relief, but these actions are often not inherently enjoyable. Relief comes from temporarily easing the anxiety or fear that something dreadful might occur if the compulsion isn’t performed. For instance, excessive handwashing can temporarily assuage the fear of contamination, but the act itself is not pleasurable; it is a response to an underlying fear.
Autistic Rituals:
In contrast, Autistic rituals typically arise from a desire for predictability and enjoyment in routine. These rituals will not have a direct cause-effect relationship with fear or anxiety, like OCD compulsions. Instead, they are often inherently satisfying or soothing. The anxiety that might arise when these rituals are disrupted is more about a break in routine or a change in what feels familiar and comforting rather than a fear that something bad will happen as a direct consequence. An Autistic individual might find a particular sensory experience or sequence of actions enjoyable or calming, and disruption to this can cause discomfort or stress.
Key Differences:
Source of Anxiety: In OCD, the anxiety is directly tied to fear-driven obsessions. In Autism, anxiety may result from a disruption in preferred routines or sensory experiences.
Emotional Response: Compulsions in OCD are often distressing and performed out of a sense of urgency or fear. Autistic rituals are typically engaged in because they are enjoyable or soothing.
Cause-Effect Relationship: OCD compulsions are driven by a belief that something bad will happen if they’re not performed. Autistic rituals are more about seeking comfort, consistency, or sensory satisfaction.
Understanding these distinctions helps in providing appropriate support and interventions. For people with OCD, the focus is on managing anxiety and breaking the cycle of compulsions. In contrast, for Autistic people, it’s important to respect our need for routine and sensory preferences, providing a stable and predictable environment that acknowledges our way of experiencing the world. So, in OCD, we’d want to target compulsion activities; in autism, we’d want to support and allow rituals (unless rituals are harmful to self or others).
Differentiating Compulsions from ADHD Compensation Strategies
Just as it can be challenging to distinguish Autistic rituals from OCD compulsions, it can also be challenging to differentiate between compulsions and ADHD compensation strategies. While some behaviors may seem superficially similar, their underlying motivations and consequences are notably different.
Compulsions in OCD:
Compulsions are anxiety-driven behaviors primarily associated with OCD. They are performed as a response to obsessive thoughts, often characterized by a fear that something bad will happen if the compulsion is not carried out. These actions, such as checking or arranging things, are typically not in themselves pleasurable but are driven by an urgent need to alleviate anxiety or prevent a feared outcome.
ADHD Compensation Strategies:
On the other hand, compensation strategies in ADHD are developed to manage challenges with executive functioning, like memory, attention, or organization. For example, a person with ADHD might adopt checking behaviors not out of a fear-driven compulsion but as a strategy to offset difficulties with memory or attention to detail. They may repeatedly check their work, appointments, or tasks because they have learned through experience that their memory or attention might not be reliable. This is more about creating systems or routines that help manage their ADHD than about responding to an obsession.
Key Differences:
Root Cause: The root of OCD compulsions is anxiety and fear from obsessions, while ADHD compensation strategies are developed to cope with executive functioning challenges.
Emotional Drive: OCD compulsions are typically driven by intense anxiety or fear, whereas ADHD compensation strategies may be influenced by emotions like frustration, stress, or a desire for efficiency. Emotions can play a significant role in the development and execution of these strategies.
Anxiety: Both OCD compulsions and ADHD compensatory strategies can trigger anxiety, but the origins of this anxiety differ slightly. When dealing with ADHD-related anxiety, you often find a clearer, more direct link. For instance, in OCD, the fear might be something like, “If I don’t count by twos when I walk, my mom will die” (yes, I had this childhood compulsion too). In contrast, with ADHD, the anxiety could stem from concerns like, “If I don’t triple-check this email, I might accidentally send it to the entire team.” If this fear arises from a history of distractibility and acts as a countermeasure to executive functioning challenges, it qualifies as an anxiety-driven compensation strategy.
It’s important to note that individuals who have both ADHD and OCD may experience compensatory strategies that incorporate elements of OCD. For example, before sending out a newsletter to my 20,000 subscribers, I will often quadruple-check the links and sometimes get stuck in a checking loop; this is both an ADHD compensatory strategy and there is some OCD checking behavior in the mix.
Understanding these nuances is key. In OCD, the therapeutic approach often involves addressing the anxiety and breaking the compulsive cycle. In ADHD, the focus might be more on outsourcing executive functioning tasks whenever possible and developing effective strategies and tools to cope with executive functioning difficulties. Recognizing these differences ensures that individuals receive the most appropriate and supportive interventions for their specific needs.
Summary and Conclusion
Navigating the world of Obsessive-Compulsive Disorder (OCD) can be a complex journey, especially when it intertwines with other aspects of neurodivergence like Autism or ADHD. Through my own experiences and those I’ve encountered in my practice, I’ve come to understand that OCD is more than just a series of rituals or habits. It’s a profound part of one’s mental landscape that requires understanding, empathy, and tailored care.
OCD manifests as persistent, intrusive thoughts (obsessions) and repetitive actions (compulsions) that can significantly impact daily life. It’s a form of neurodivergence that, although it may persist through life, can be managed effectively with the right support. The intersection of OCD with other neurodiverse conditions like ADHD and Autism adds layers to the challenges faced by individuals. Recognizing this overlap is crucial in providing comprehensive care that addresses the whole person.
In my journey, both personal and professional, I’ve learned that the way we talk about and understand our mental health deeply affects our approach to treatment and care. Whether we say we ‘have OCD’ or consider it part of our neurotype, what matters most is finding a narrative that feels right for us and allows us to approach our challenges with hope and resilience.
* Footnote: Further complicating the debate on the nature of OCD within the spectrum of neurodivergence is the fact that about 50% of individuals diagnosed with OCD will experience persistent symptoms throughout their lives. These symptoms often fluctuate, intensifying during periods of increased anxiety. This observation raises a pivotal question: Is OCD an inherent neurotype, or is it a situational form of neurodivergence? Does it represent a permanent aspect of an individual’s neurological makeup, or is it a condition that one might have at certain times and not at others? Such questions underscore not only the complexity of OCD but perhaps also the complexity of the entire framework of neurotypes and neurodivergence in general. This highlights the importance of considering individual experiences and the diverse spectrum of neurodiversity when understanding conditions like OCD.
References
Brem, S., Grünblatt, E., Drechsler, R., Riederer, P., & Walitza, S. (2014). The neurobiological link between OCD and ADHD. Attention deficit and hyperactivity disorders, 6(3), 175–202. =
Masi G, Millepiedi S, Mucci M, Bertini N, Pfanner C, Arcangeli F. Comorbidity of obsessive-compulsive disorder and attention-deficit/hyperactivity disorder in referred children and adolescents. Compr Psychiatry. 2006;47(1):42–47.
Masi G, Millepiedi S, Perugi G, Pfanner C, Berloffa S, Pari C, Mucci M, Akiskal HS. A naturalistic exploratory study of the impact of demographic, phenotypic, and comorbid features in pediatric obsessive-compulsive disorder. Psychopathology. 2010;43(2):69–78.
Yuhas, Daisy, Untangling the ties between autism and obsessive-compulsive disorder, Spectrum News.
Ziegler, S., Bednasch, K., Baldofski, S., & Rummel-Kluge, C. (2021). Long durations from symptom onset to diagnosis and from diagnosis to treatment in obsessive-compulsive disorder: A retrospective self-report study. PloS one, 16(12), e0261169.