DSM-5 Picture Series
Welcome to another installment of our DSM-5 in Pictures series! This series aims to break down complex diagnostic criteria into visual and digestible understandings and to demystify the often intimidating world of mental health diagnoses. Too often, people are given diagnoses that they don’t understand and lack someone to help explain what it all means.
This is especially true in the case of PTSD (Post-Traumatic Stress Disorder). PTSD is so much more than experiencing symptoms X, Y, and Z. Instead, PTSD helps explain how and why your body got stuck in the trauma. Once you have this lens, you can begin moving toward how to get unstuck.
So today, we’re diving into Post-Traumatic Stress Disorder (PTSD), a condition that affects many but is often misunderstood.
What is PTSD?
PTSD is a mental health condition that can develop after a person experiences or witnesses a traumatic event. These events may include but are not limited to exposure to actual or threatened death, serious injury, or sexual violence. It is important to note that while many individuals experience trauma, not all will develop PTSD. On average, only about 1 in 3 people who experience severe trauma will go on to develop PTSD (NHS).
Why Do Some People Develop PTSD?
Some people are more vulnerable to developing PTSD than others. Factors that can increase the risk of developing PTSD include: having a sensitive neurological or nervous system (such as in autism and ADHD); a history of depression, anxiety, or other mental health condition; and having limited social support. These vulnerabilities affect how one processes and recovers from traumatic experiences, making it more challenging to return to a personal baseline (NHS).
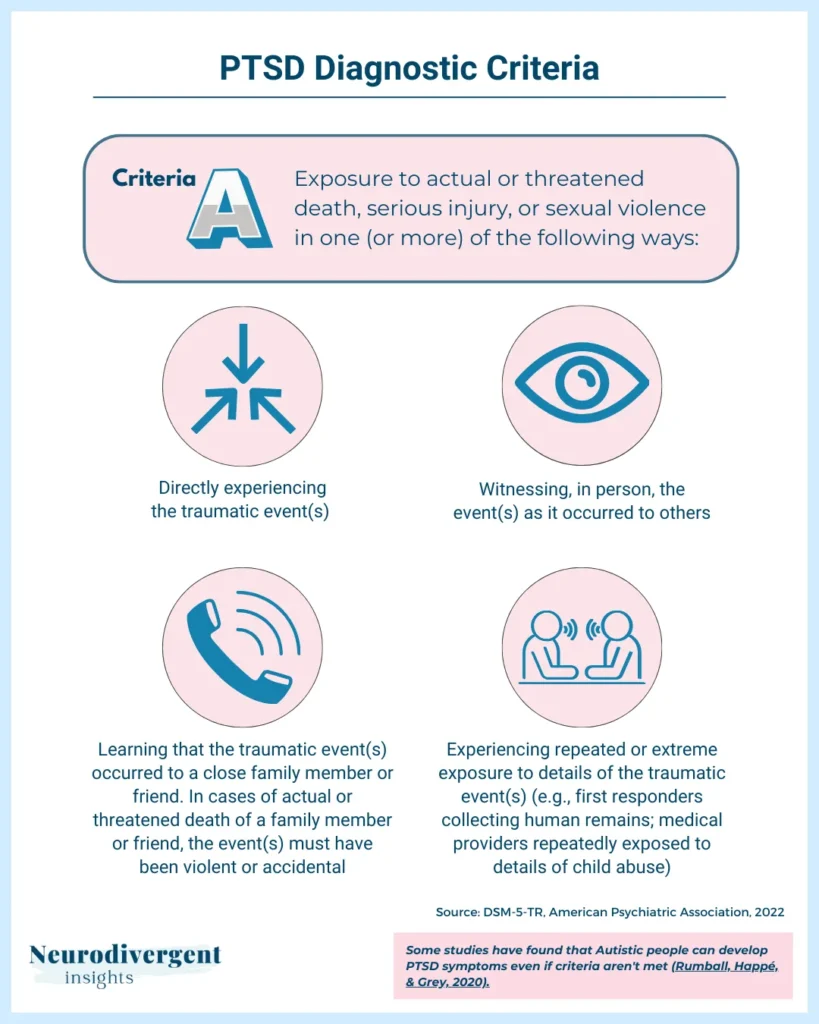
Certain groups, such as Autistic people, are at such a heightened risk that they can develop PTSD symptoms even when Criterion A (direct exposure to traumatic events) is not met. Essentially, they can develop PTSD from “lesser” traumas due to their greater sensitivity to stress and difficulty in processing traumatic experiences (Rumball et al., 2020). You can read more about the intersection of autism and PTSD here, and ADHD and trauma here.
Conceptualizing PTSD
While the clinical definition and symptoms of PTSD are useful, it can also be helpful to zoom out and conceptualize PTSD in broader terms. PTSD can be seen as a condition where the body and mind are stuck in a state of trauma, unable to move forward. The mind is hijacked by flashbacks, ruminations on the event, and overly catastrophic beliefs about oneself and the world. The body does not recognize that the trauma has ended and the stress response remains activated. Familiar smells, sounds, or sights that resemble the traumatic event can trigger a return to the traumatic state. The person experiences a fragmented existence with parts of their psyche still caught in the trauma.
One theory is that this happens as a safety mechanism gone awry. For example, hypervigilance in PTSD serves to keep the individual on high alert to avoid future threats or to be ready to react quickly should danger arise again. Flashbacks and rumination might serve the purpose of forcing the person to repeatedly process the traumatic event in an attempt to make sense of it and prepare for potential future occurrences.
The negative beliefs about oneself and the world (e.g., “the world is not safe”) also function as protective mechanisms. These beliefs can help the individual avoid perceived dangers but also contribute to a pervasive sense of fear and helplessness.
When survival mechanisms which began as protective responses to keep us safe become ingrained habits, they may no longer help us. Instead, they can cause significant stress and pain. Viewing PTSD as a condition where our natural survival instincts have gone awry helps explain why people with PTSD struggle to feel safe and at ease in their daily lives. Their bodies and minds are constantly on high alert, trying to protect them.
Core Features of PTSD
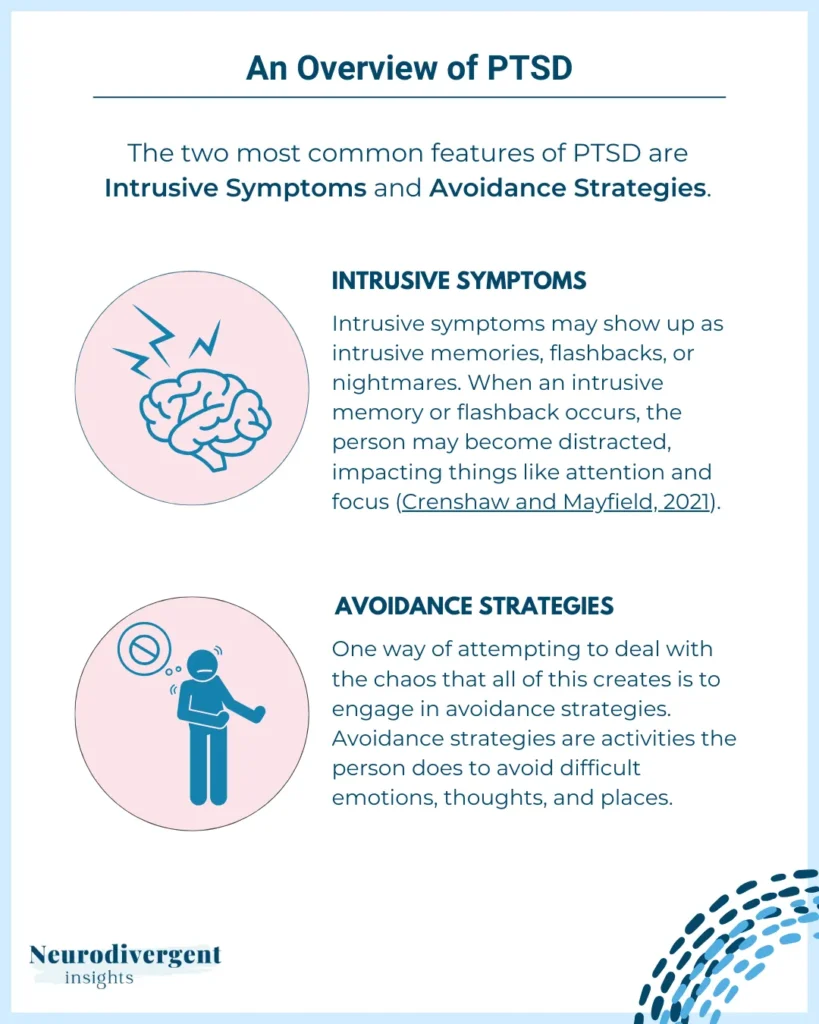
Now that we have a framework for understanding PTSD—when we become stuck in trauma as a result of a faulty safety mechanism—we can dive into the core features of PTSD. The two most common features of PTSD are:
Intrusive Symptoms
Intrusive symptoms are particularly disruptive, as they involve unwanted and distressing memories, flashbacks, or nightmares that can severely affect a person’s ability to focus and function normally. This helps explain why individuals with PTSD might struggle with attention and concentration in their daily activities.
Avoidance
Avoidance is a common coping mechanism that people with PTSD use to manage their symptoms. By avoiding reminders of the trauma, whether they are internal (emotions, memories) or external (places, people), individuals may attempt to shield themselves from distress; but, this can lead to increased isolation and further difficulty processing the traumatic event.
PTSD Diagnostic Criteria Breakdown
Having explored the core features of PTSD, we can now look at how these experiences fit into the specific diagnostic criteria set out in the DSM-5. The DSM-5 organizes PTSD criteria into several categories as Criteria A, B, C, D, and E. Here’s a simplified visual representation:
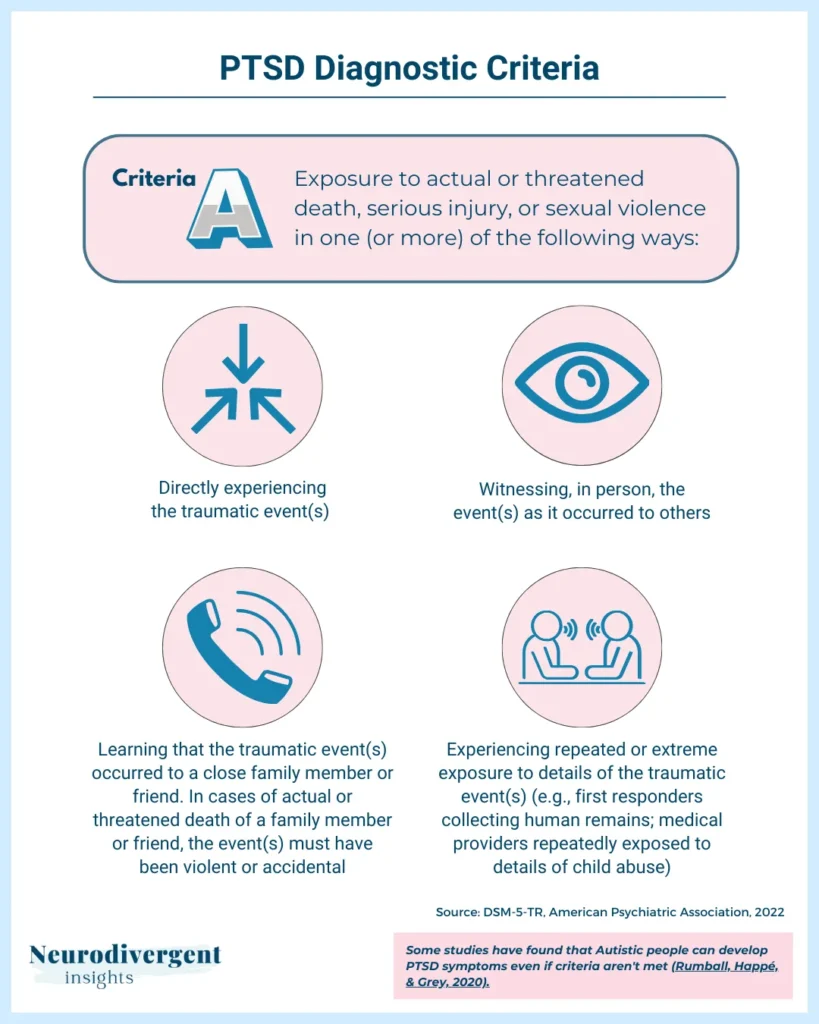
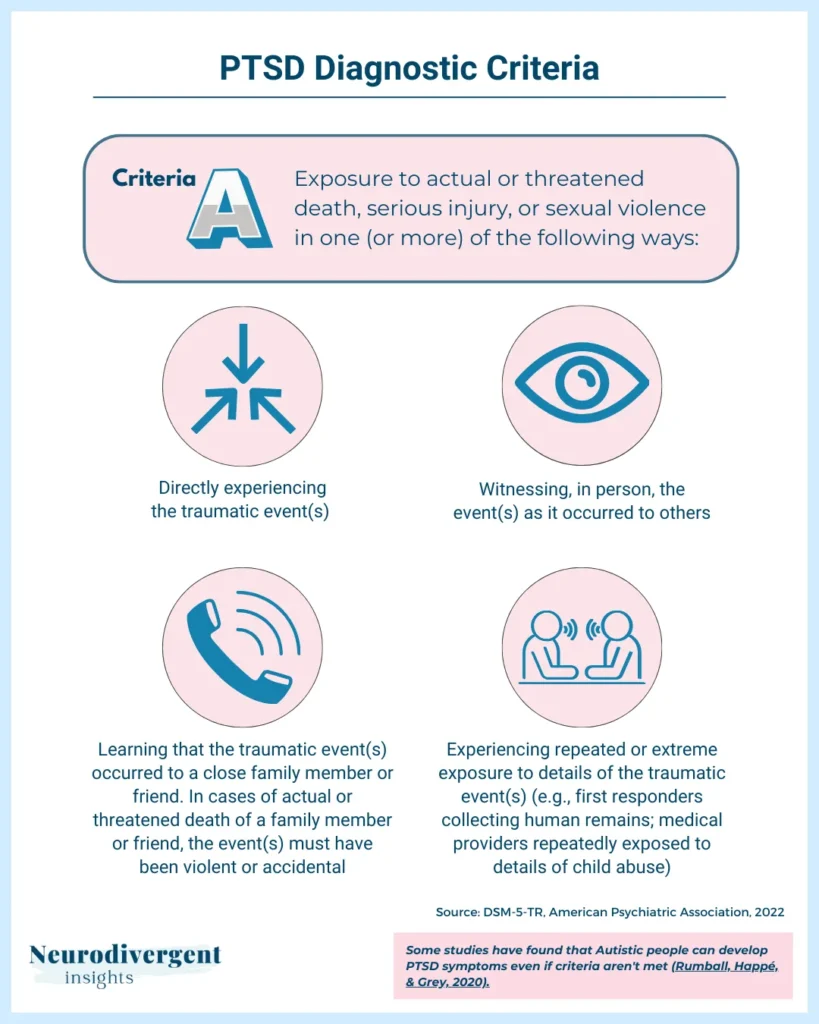
PTSD Criteria A: Stressor
To meet Criteria A, an individual must have been exposed to a traumatic event in one or more of the following ways:
Direct Exposure: Personally experiencing the traumatic event.
Witnessing the Event in Person: Seeing the traumatic event happen to others.
Learning About Trauma: Discovering that a close relative or friend experienced a traumatic event. In cases of actual or threatened death of a family member or friend, the event must have been violent or accidental.
Indirect Exposure: Repeated or extreme exposure to aversive details of the traumatic event, typically in the course of professional duties (e.g., first responders, medical personnel). Note: Criterion 4 does not apply to exposure through electronic media, television, movies, or pictures, unless this exposure is work related.
Common events that can lead to PTSD include:
Serious Accidents: Involvement in severe car accidents, workplace accidents, or other types of serious accidents.
Physical or Sexual Assault: Experiencing or witnessing physical violence or sexual assault.
Abuse: Enduring or witnessing abuse, including childhood abuse or domestic violence.
Exposure to Traumatic Events at Work: Encountering traumatic situations as part of one’s job, such as emergency responders or military personnel. This also includes remote exposure, such as viewing graphic content as part of one’s professional duties.
Serious Health Problems: Facing severe health issues, such as being admitted to intensive care, which can be traumatic.
Childbirth Experiences: Traumatic events related to childbirth, such as losing a baby or experiencing life-threatening complications.
The Death of Someone Close: The unexpected or violent death of a loved one.
War and Conflict: Exposure to combat or being in a war zone.
Torture: Experiencing or witnessing acts of torture.
Source: (DSM-5-TR, American Psychiatric Association, 2022)
These events can overwhelm a person’s ability to cope, leading to the development of PTSD.
PTSD Criteria B: Intrusion Symptoms
Intrusion symptoms are one of the core features of PTSD — the traumatic event persistently invades the present moment. To meet Criteria B, an individual must experience one or more of the following symptoms:
Recurrent, Involuntary, and Intrusive Memories:
Unwanted, distressing memories of the traumatic event that repeatedly and involuntarily come to mind.
Traumatic Nightmares:
Frightening dreams that involve the traumatic event or themes related to it, causing significant distress and often disrupting sleep.
Dissociative Reactions (e.g., Flashbacks):
Episodes where the individual feels or acts as if the traumatic event is happening again. During flashbacks, the person may lose awareness of their current surroundings and re-experience the traumatic event as if it were occurring in the present moment.
Intense or Prolonged Distress After Exposure to Traumatic Reminders:
Severe emotional distress when encountering internal or external cues that symbolize or resemble aspects of the traumatic event. These reminders can trigger intense feelings of fear, helplessness, or horror.
Marked Physiological Reactivity After Exposure to Trauma-Related Stimuli:
Significant physical reactions (e.g., increased heart rate, sweating, or trembling) in response to cues that remind the individual of the traumatic event. These physiological responses are part of the body’s fight-or-flight mechanism and can occur even when there is no real danger.
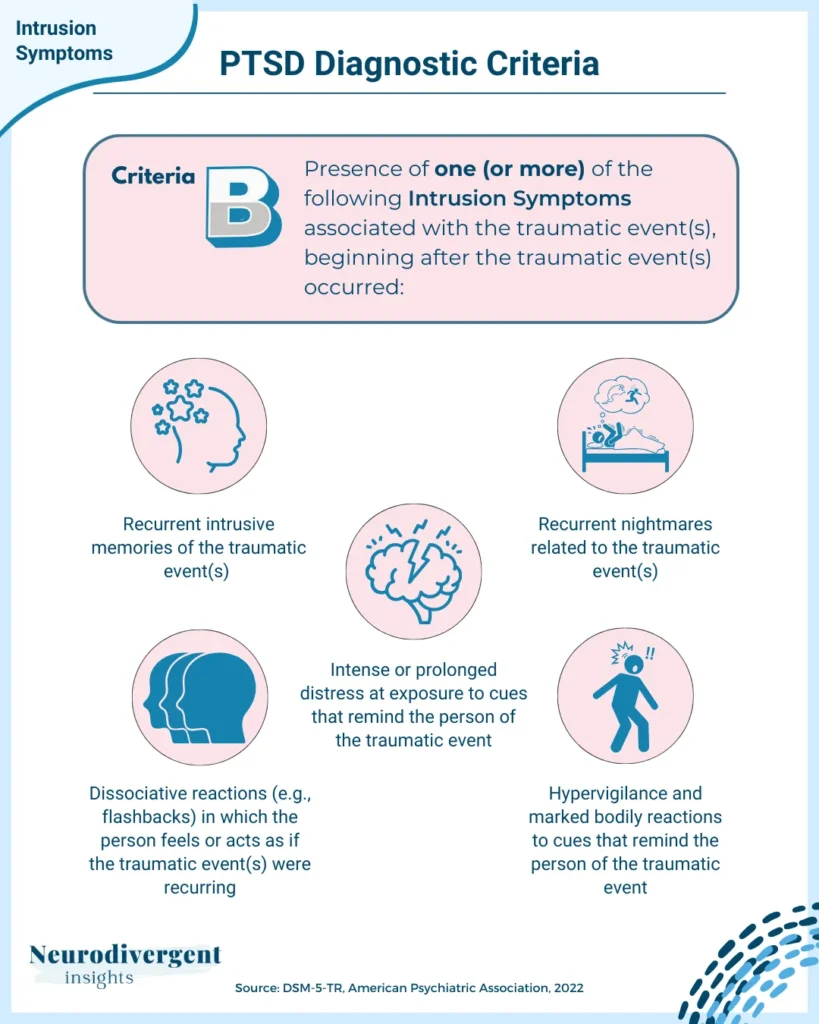
Source: (DSM-5-TR, American Psychiatric Association, 2022)
The intrusive symptoms of PTSD highlight how deeply trauma can embed itself in a person’s mind and body, continuously affecting their day-to-day lives.
Criteria C: Avoidance
Avoidance symptoms are behaviors and actions that individuals with PTSD use to escape reminders of their traumatic experiences. To meet Criteria C, an individual must exhibit at least one of the following symptoms that began after the traumatic event(s):
Efforts to Avoid Distressing Trauma-Related Memories, Thoughts or Feelings:
Deliberate attempts to steer clear of thoughts, memories, or emotions associated with the traumatic event. This can include using distractions or mental strategies to suppress these distressing thoughts and feelings.
Efforts to Avoid External Reminders:
Active avoidance of people, places, conversations, activities, objects, smells, or situations that trigger distressing thoughts or feelings about the trauma. This might involve significant changes in daily routines, social withdrawal, or avoiding certain locations to prevent reminders of the traumatic experience.
Source: (DSM-5-TR, American Psychiatric Association, 2022)

These avoidance behaviors start as attempts to reduce distress and maintain control, but they can lead to increased isolation and difficulty processing the traumatic event. A person can easily fall into the avoidant-anxious loop, where the more they avoid triggers, the more their anxiety grows, allowing PTSD and the trauma to take over more aspects of their life. Consequently, their world becomes incredibly small. Additionally, relying on avoidance as a coping mechanism decreases their tolerance for triggers, making them more easily triggered in their day-to-day life. This is one of the reasons avoidance behaviors are often addressed as part of PTSD treatment.
Criteria D: Negative Alterations in Cognitions and Mood
These avoidance behaviors start as attempts to reduce distress and maintain control, but they can lead to increased isolation and difficulty processing the traumatic event. A person can easily fall into the avoidant-anxious loop, where the more they avoid triggers, the more their anxiety grows, allowing PTSD and the trauma to take over more aspects of their life. Consequently, their world becomes incredibly small. Additionally, relying on avoidance as a coping mechanism decreases their tolerance for triggers, making them more easily triggered in their day-to-day life. This is one of the reasons avoidance behaviors are often addressed as part of PTSD treatment.
Inability to Recall Key Features of the Traumatic Event:
Difficulty remembering important aspects of the traumatic experience, not due to head injury, alcohol, or drugs, but rather the mind’s way of coping with extreme stress.
Persistent Negative Beliefs and Expectations:
Ongoing and often distorted negative thoughts about oneself, others, or the world (e.g., “I am bad,” “No one can be trusted,” “The world is completely dangerous”).
Distorted Blame:
Unjustly blaming oneself or others for causing the traumatic event or its consequences, which can intensify feelings of guilt and shame.
Persistent Negative Emotions:
Enduring feelings of fear, horror, anger, guilt, or shame that are directly related to the traumatic experience and persist long after the event.
Diminished Interest in Significant Activities:
A noticeable decline in interest or participation in activities that were once significant or enjoyable, leading to a sense of disconnection from one’s previous life.
Feeling Alienated from Others:
Experiencing a sense of detachment or estrangement from other people, often feeling unable to connect or relate to others as before.
Constricted Affect:
Persistent inability to experience positive emotions such as happiness, love, or satisfaction, resulting in a muted or blunted emotional state.
Source: (DSM-5-TR, American Psychiatric Association, 2022)
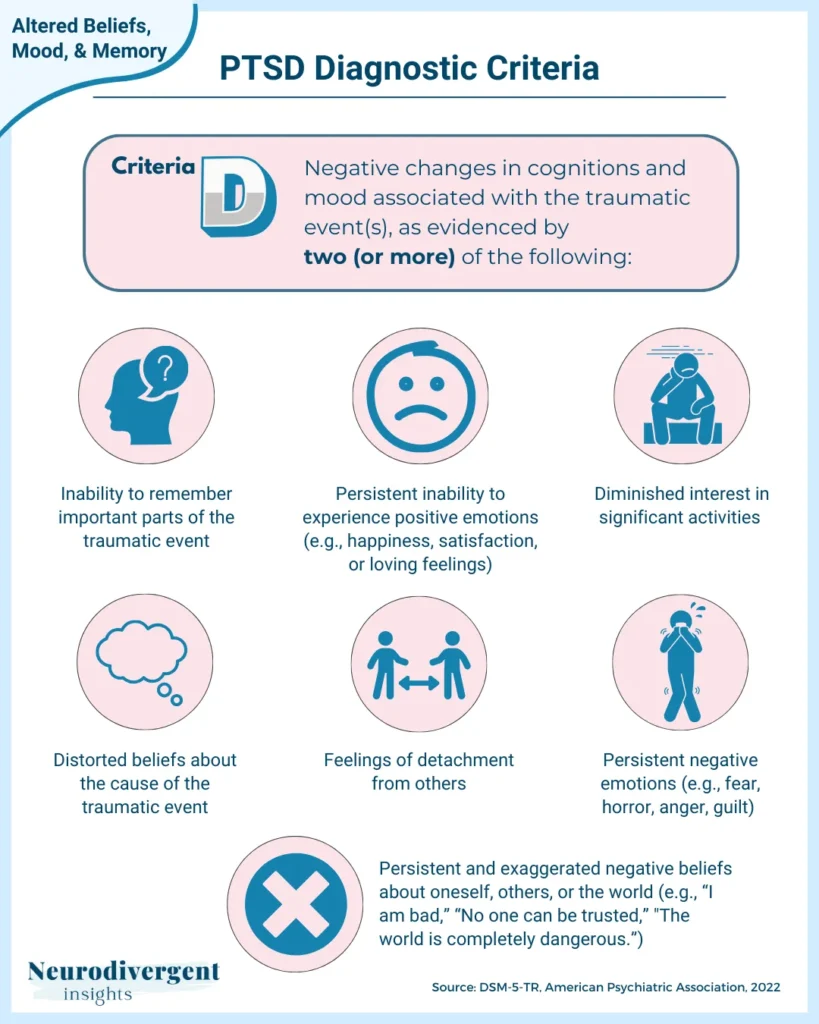
These symptoms show how PTSD can deeply change a person’s thoughts and feelings, making it hard to feel normal or connect with others again. Recognizing these changes is essential to fully understand the impact of PTSD on mental health.
Criteria E: Alterations in Arousal and Reactivity
Irritable or Aggressive Behavior:
Increased irritability, angry outbursts, or aggressive behavior, often disproportionate to the situation and sometimes directed towards people or objects.
Self-Destructive or Reckless Behavior:
Engaging in behaviors that are harmful or risky, such as substance abuse, reckless driving, or other activities that could lead to injury or harm.
Hypervigilance:
An enhanced state of sensory sensitivity and an exaggerated intensity of behaviors intended to detect threats. This can lead to a constant state of alertness, making it difficult to relax or feel safe.
Exaggerated Startle Response:
A heightened reaction to unexpected stimuli, such as loud noises or sudden movements, often resulting in an intense physical and emotional response.
Problems in Concentration:
Difficulty focusing or maintaining attention on tasks, which can affect daily functioning, work performance, and academic achievement.
Sleep Disturbance:
Trouble falling or staying asleep, restless or unsatisfying sleep, and frequent waking throughout the night. Nightmares and anxiety can further disrupt sleep patterns.
Source: (DSM-5-TR, American Psychiatric Association, 2022)
These symptoms show how PTSD affects the nervous system, putting it in a constant state of high alert. It’s like the wiring around the amygdala (the brain’s alarm bell) becomes extra sensitive, keeping the brain always ready for potential threats. This heightened state of arousal can be exhausting and overwhelming, making it hard for a person to live their life normally and enjoy day-to-day activities.
Note: In addition to these symptoms, some individuals with PTSD may exhibit a “freeze” response. This survival mechanism is characterized by feeling paralyzed or unable to take action when faced with a threat. The freeze response is another way the brain and body attempt to cope with trauma.
Criteria F-H
To diagnose PTSD accurately, it’s important to ensure that the symptoms are persistent, impactful, and not caused by other factors. Criteria F-H help differentiate PTSD from other conditions and temporary reactions to trauma.
Criteria F: Duration
The symptoms must persist for more than one month after the traumatic event. This duration helps distinguish PTSD from acute stress disorder, which has similar symptoms but a shorter duration. If a person is assessed within the first 30 days, they may initially be diagnosed with acute stress disorder. However, if the symptoms persist beyond 30 days, the diagnosis will be changed to PTSD.
Criteria G: Impact
The symptoms must cause significant distress or impairment in daily life, including social relationships, work, school, or other important areas. This impact highlights the severity of PTSD and its effect on the individual’s ability to function normally.
Criteria H: Exclusion
The symptoms cannot be attributed to the effects of medication, drugs, or other medical conditions. This ensures that the diagnosis of PTSD is accurate and not confused with symptoms caused by substance use or other health issues.
These criteria emphasize the need for persistent symptoms, a significant impact on daily life, and ruling out other potential causes.
If You've Been Diagnosed: What's Next?
As someone who has experienced and recovered from PTSD, I understand how overwhelming it can be. Receiving a PTSD diagnosis can feel daunting, but it’s an important step toward managing your symptoms and finding your way back to a more balanced state. Once you have a diagnosis you have a better understanding of what your mind and body are going through. Here are some things to do after your diagnosis:
1. Seek Professional Help
While PTSD can be incredibly challenging, the good news is that it responds well to treatment.
Therapy: Consider evidence-based treatments like Cognitive Processing Therapy (CPT), Eye Movement Desensitization and Reprocessing (EMDR), Narrative Exposure Therapy (NET), Trauma-Focused Cognitive Behavioral Therapy (TF-CBT), or Acceptance and Commitment Therapy (ACT). Somatic-based approaches like Sensorimotor Psychotherapy are also effective. Additionally, you might explore modalities like Internal Family Systems (IFS) Therapy, with which many Autistic and ADHD people connect.
Medication: Talk to a psychiatrist about medications that can help manage your symptoms and calm down your overactive sympathetic nervous system.
2. Build a Support System
It’s tempting to withdraw when experiencing PTSD, but that’s when we need our support team more than ever. Even though it might feel counterintuitive, it’s important to cultivate and develop your support system.
Friends and Family: Identify and lean on friends and family members you can trust for emotional support.
Support Groups: Consider joining an online or in-person PTSD support group to connect with others who understand your experience. Be mindful of where you are in your healing journey, as some groups may be re-triggering. Joining a group facilitated by a professional therapist can help create a safe environment.
3. Educate Yourself
Understanding what is happening to your body and mind is one of the most empowering steps in managing PTSD. Knowing the science behind your symptoms can make these moments less scary and help you regain a sense of control.
Learn About PTSD: Understanding PTSD can empower you and reduce feelings of helplessness. Knowing how PTSD impacts your nervous system and mind can help you regain a sense of control. This is especially important for Autistic people.
Identify Triggers and Avoidance Patterns: Recognizing your triggers and avoidance behaviors can help you manage them with more agency.
4. Develop Coping Strategies
You’ll need a toolkit of coping strategies to help pull you out of flashbacks and intrusive memories, as well as to settle an overactive nervous system. Here are some coping strategy buckets to consider:
Mindfulness, Relaxation, and Grounding: Practices like meditation, deep breathing, and yoga can help reduce stress.
Healthy Lifestyle: Maintain a balanced diet, exercise regularly, and ensure good sleep to support your nervous system and build resilience.
5. Create a Safety Plan
With PTSD, we are more prone to reckless and dangerous outbursts. Having a plan in place for these moments helps keep us safe and protects us from those impulsive moments.
Crisis Plan: Develop a plan for overwhelming moments, including emergency contacts, safe places, and grounding techniques that work for you.
Seek Joy: Regularly engage in activities that bring you joy, meaning, and relaxation.
6. Monitor Your Progress
When it comes to PTSD, slow and steady wins the race. Tracking your progress in a visual and concrete way can be empowering and help keep you motivated.
Track Symptoms: Keep a journal of your symptoms to monitor progress and identify patterns. Healing can feel slow day to day, but tracking your progress over 30 days can be revealing. Your therapist may use tools like the PTSD Screener (PCL-5) to measure your progress. (Scroll to the bottom of this page for downloadable measures.)
Regular Check-ins: Have regular appointments with your therapist or doctor to adjust your treatment plan as needed.
7. Be Gentle with Yourself
Many of us become particularly punitive and harsh with ourselves in the context of PTSD. Be gentle, both with yourself and the process!
Healing Takes Time: Recovery is gradual, so be kind and patient with yourself.
Celebrate Small Wins: Acknowledge and celebrate every step forward.
8. Seek Joy And Meaning
Regularly engaging in activities that bring you joy, meaning, and relaxation can significantly increase your resilience as you navigate PTSD healing.
Conclusion
PTSD is a mental health condition that develops after experiencing or witnessing a traumatic event. It’s important to understand the core features of PTSD, which include intrusive symptoms, avoidance behaviors, negative changes in cognition and mood, and heightened arousal and reactivity. The DSM-5 criteria for diagnosing PTSD ensure that symptoms last for more than a month, cause significant distress or impairment, and aren’t due to other medical conditions.
Fortunately, there are effective treatments available. These include approaches like Cognitive Processing Therapy (CPT), Eye Movement Desensitization and Reprocessing (EMDR), and Somatic-based approaches. Building a strong support system, developing coping strategies, and seeking professional help are key steps for managing PTSD. With the right treatment and support, you can make progress toward recovery and healing.
References
National Health Service. (n.d.). Causes – Post-traumatic stress disorder (PTSD). NHS. https://www.nhs.uk/mental-health/conditions/post-traumatic-stress-disorder-ptsd/causes/
Rumball, F., Happé, F., & Grey, N. (2020). Experience of trauma and PTSD symptoms in autistic adults: Risk of PTSD development following DSM‐5 and non‐DSM‐5 traumatic life events. Autism Research, 13(12), 2122-2132.
American Psychiatric Association. (2022). Diagnostic and statistical manual of mental disorders (5th ed., text rev.). American Psychiatric Publishing.