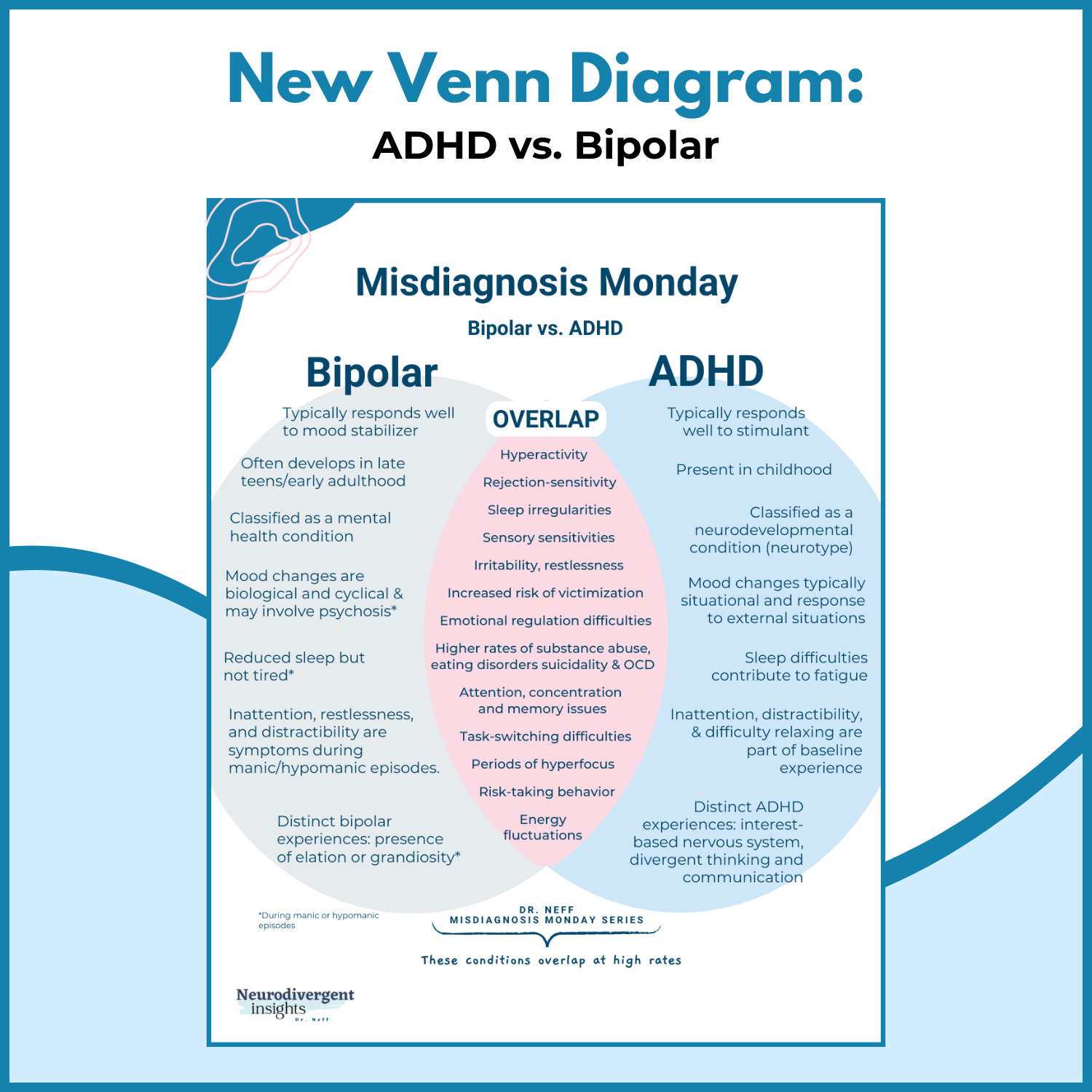
ADHD vs. Bipolar
After wrapping my 10-week series on Autism, this is my first week taking on ADHD and common co-occurring conditions/misdiagnoses. Similar to Autism, ADHD can be difficult to diagnose, leading to a missed diagnosis or misdiagnosis of ADHD. While there is a perception that ADHD is overdiagnosed, Schiweck et al., 2021 suggest the opposite may be true.
The presentation of ADHD in adults is often poorly understood, making adults with undiagnosed ADHD vulnerable to being diagnosed and treated for co-occurring mood disorders while their ADHD is missed (Schiweck et al., 2021). When the underlying ADHD is diagnosed and treated, the mood symptoms often improve. So why a ten-week series on ADHD and misdiagnoses? To answer this question, let me borrow the words of Schiweck et al., 2021:
“Studies have concluded that emotional dysregulation is a distinctive attribute of adult ADHD psychopathology. However, these symptoms may be misdiagnosed as a mood disorder. Similarly, ADHD symptoms may be masked by substance use. Physicians are often more familiar with mood and anxiety disorders, which may contribute to misdiagnosis and delays in treating ADHD in adults. It has been suggested that stress, depression, and anxiety could manifest as a consequence of undiagnosed and untreated ADHD.”
The most common co-occurring conditions with ADHD include depression, anxiety disorders, bipolar disorder, SUDs, and personality disorders (Schiweck et al., 2021).
Over the next ten weeks, I will cover these and other common co-occurring conditions. It is essential to understand and detect undiagnosed ADHD when it is present because when ADHD is co-occurring with these disorders, treating the ADHD has been shown to improve symptoms of the co-occurring disorders (SUD, bipolar, depression, and anxiety) Katzman et al., 2017).
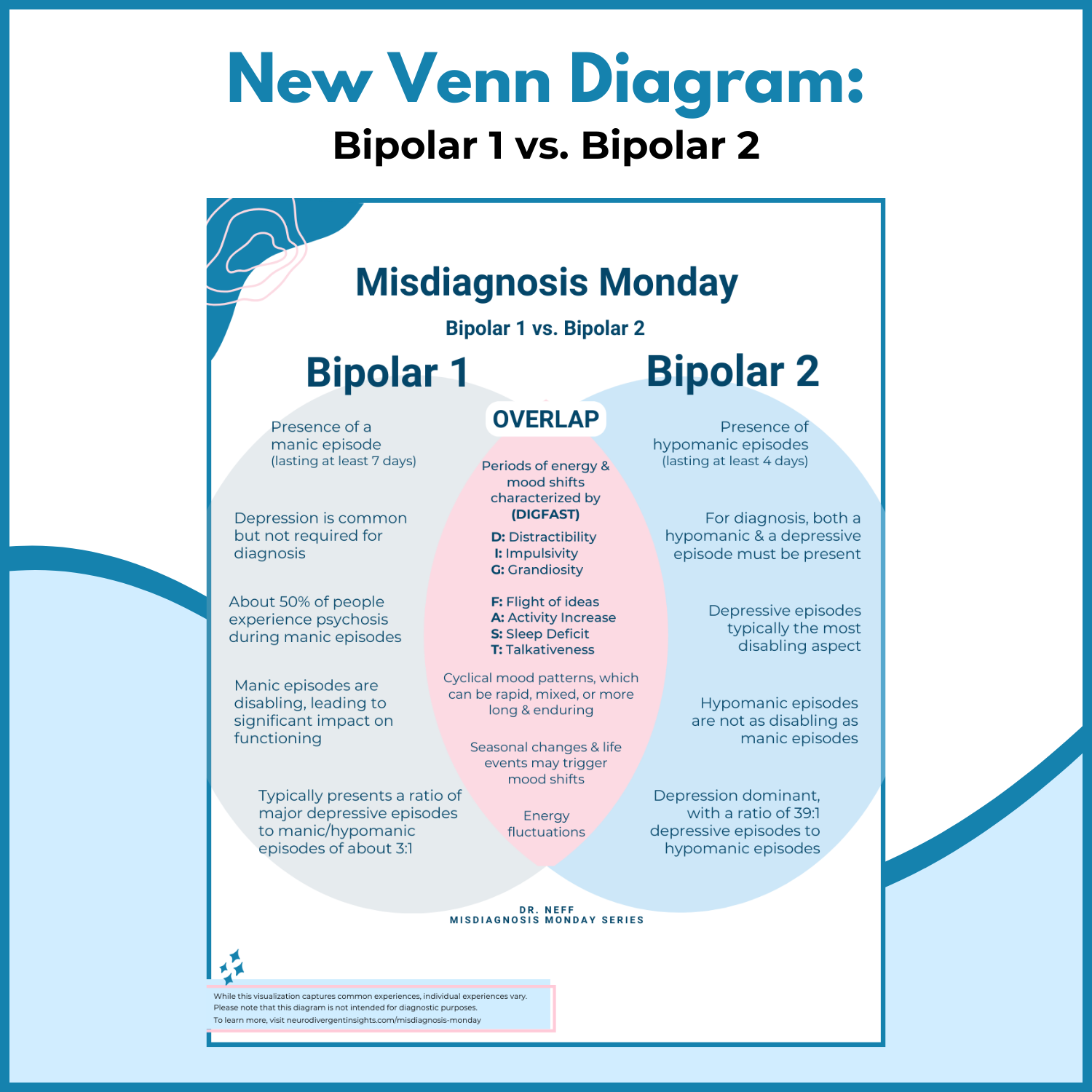
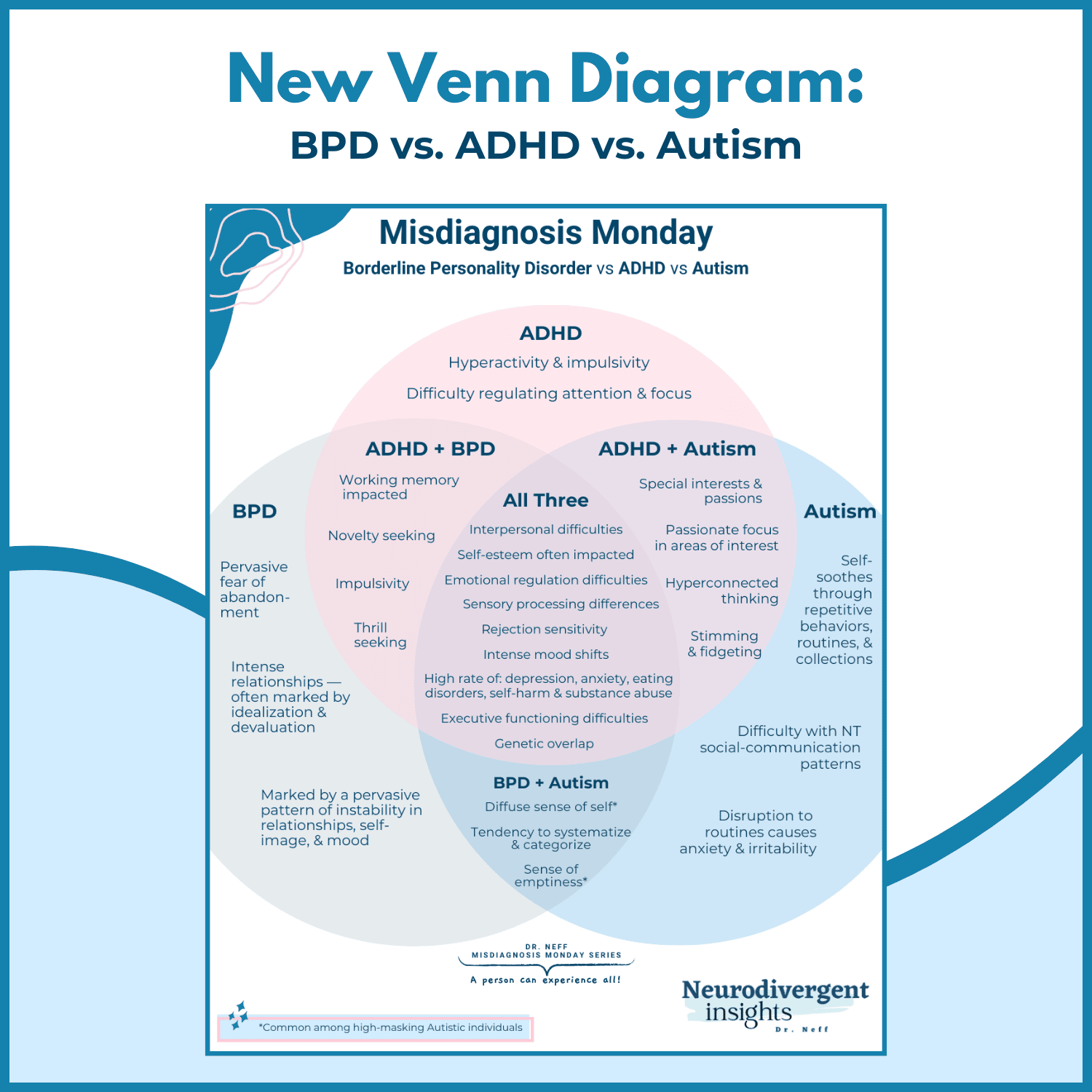
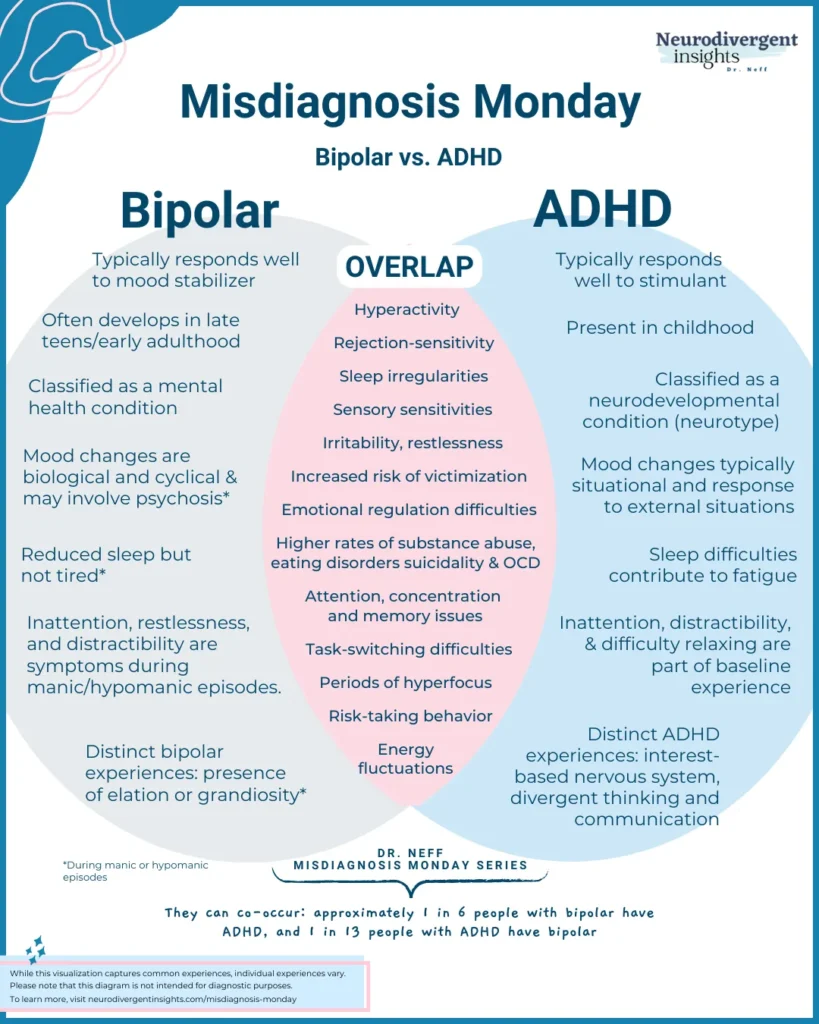
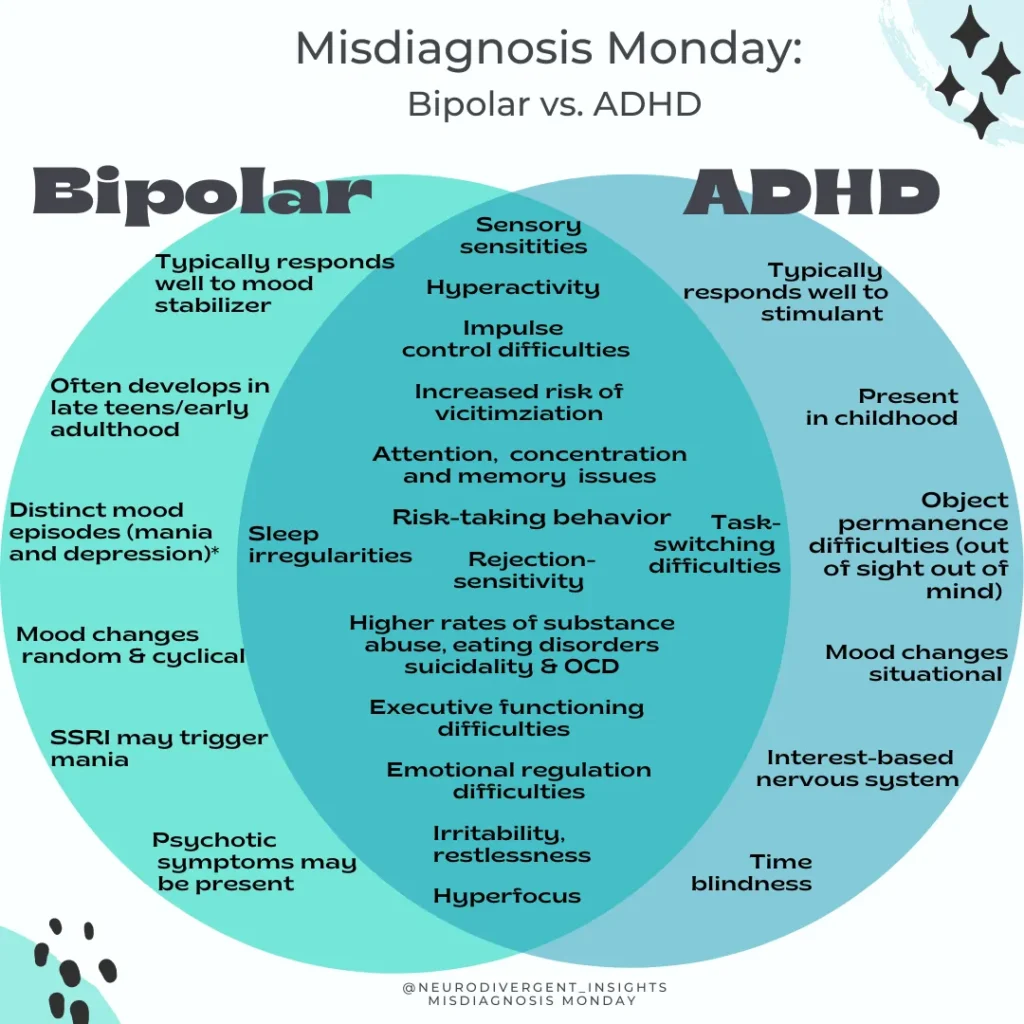
ADHD and Bipolar
ADHD and Bipolar can be tough to distinguish from one another as there are many overlapping symptoms/traits/experiences. It is essential to distinguish them from one another as the treatment of these conditions is very different and requires different pharmaceutical interventions.
While misdiagnosis indeed occurs (and there is evidence to suggest ADHD children may be misdiagnosed with bipolar at elevated rates), what may happen even more is having one diagnosis missed (when a person has both). Living with both is complex and needs close monitoring. According to Schiweck et al., 2021 when they co-occur-the, one diagnosis is often missed.
Here is some data to get us started:
Prevalence of Bipolar
Approximately 10 million people in the US have Bipolar (BD)
ADHD prevalence of 5-8%
Bipolar prevalence 1-3%
Rates of Co-occurrence
(Source: Schiweck et al., 2021)
A meta-study that looked at multiple countries found a co-occurrence rate of 5.1-47.1% (co-occurring rates were highest in the U.S.)
The U.S. co-occurrence rate was 12.64
1 in 13 people with ADHD has comorbid B.D.
1 in 6 people with B.D. have ADHD
ADHD patients are at elevated risk for B.D. and first-degree relatives of B.D. Patients are at elevated risk for ADHD.
Implications of Co-occurrence
(Source for data: Schiweck et al., 2021)
The onset of bipolar symptoms nearly five years earlier in people with co-occurring ADHD
When they co-occur, one diagnosis is often missed
Early diagnosis and treatment of ADHD help reduce risks associated with both conditions
There is some evidence that early treatment of ADHD can protect from the development of future depression, bipolar, and substance abuse. Individuals with ADHD who received stimulant treatment in childhood had lower depression and bipolar disorder rates later in life compared with individuals who were not treated (Katzman et al., 2017)
Increased risk of other co-occurring mental health dx and substance abuse disorders
People who have both ADHD and B.D. have more severe ADHD symptoms and an earlier onset of B.D. symptoms Schiweck et al., 2021)
Many have been diagnosed with ODD; a higher percentage are male
People with both have more frequent episodes of mania and depression and higher instances of additional comorbid psychiatric conditions, including anxiety and substance use disorders Schiweck et al., 2021)
Co-occurrence has implications for medications (see the end of the article for specifics).
Brief Overview of Bipolar and ADHD
Bipolar 101
Bipolar, like ADHD, is considered a form of neurodivergence. Bipolar is characterized by distinct mood swings between mania and depression. Moods may cycle quite rapidly or be more prolonged and distinct from one another. Some mood episodes will have “mixed features” where they experience both elements of “highs” and “lows” within a single episode or have rapid cycles of highs/lows. Hallucinations may be present during mania. Approximately 2.8-4.4% of the U.S population has some form of bipolar within their lifetime (NIH)
Symptoms of Bipolar Disorder:
Distinct manic episodes
Hypomanic episodes (similar to mania but generally shorter episodes and can feel more manageable)
Depressive episodes
Mixed episodes (both symptoms of mania and depression are present at the same time or in rapid succession)
Psychotic symptoms (typically during mania, not everyone experiences this)
Mania
Mania is characterized by eurphia, decreased need for sleep, a sense of grandiosity, and increased risk behavior. A person may also experience increased agitation, irritability, hypervigilance (jumpy), increased sensory sensitivities, and may experience psychotic symptoms (hallucinations and delusions). Hypomania is similar to mania but in a less intense version. Symptoms of mania include:
More energized than usual despite a reduced desire and ability to sleep
Feeling so hyper that person doesn’t act like their usual self
Experiencing rapid shifting ideas, uncontrollable racing thoughts, or quickly changing topics when speaking
Excessive talking/speaking faster than typically
More social and outgoing than typical
Increased self-confidence and grandiosity (feeling invincible or on top of the world)
An increase in activity levels, engagement, or restlessness. The person may work on multiple projects simultaneously
An increase in irritability and aggression may be present
Pressured speech (increased or faster than usual)
Engaging in risky behaviors (risky driving, sexual practices, substances, or spending)
Increased impulsivity (related to spending, sex, and substances)
Hallucinations (less common)
Symptoms Associated with Bipolar Depression
Reduced or loss of interest in activities previously enjoyed
Unexplained fatigue and exhaustion
Feeling intense, overwhelmingly sadness, hopelessness, and worthlessness
Changes in sleep and appetite
Difficulty concentrating and focusing (executive functioning difficulties
Thoughts of suicide and death
ADHD 101
A Neurodevelopmental difference that is present since childhood and has a strong genetic component. ADHD traits will appear in childhood; however, may not become noticeable until stressors outweigh compensatory strategies. Following are the diagnostic criteria for ADHD (according to the DSM).
ADHD-Inattention Type
To meet diagnostic criteria, a person must have 6 of the nine traits present in childhood—before age 12—and must continue to cause difficulty in more than one environment-for example, at home and work or home and school.
1) Overlooking details
2) Task inattention
3) Appearing not to listen/difficulty listening
4) Failing to finish tasks
5) Difficulty organizing tasks,
6) Avoidance of tasks that require sustained mental activity
7) Tendency to lose things
8) Distractibility
9) Being forgetful during daily living activities.
ADHD-Hyperactivity Type
To meet diagnostic criteria, a person must have 6 of the nine traits present in childhood—before age 12—and must continue to cause difficulty in more than one environment-for example, at home and work or home and school.
1) ) Fidgeting
2) ) A tendency to leave their seat when it’s expected to sit
3)) Feeling restless
4) Difficulty maintaining quiet
5) Hyperactivity
6) Excessive talking and difficulty picking up social cues
7) Interrupting others
8) Struggles with turn-taking
9) Interrupts or intrudes on other people/other people’s possessions
Overlap Experiences and How to Spot the Difference
Mood Flux
Neurodivergent Mood fluctuations are common within the context of ADHD, which may look like bipolar mood fluctuations.
How to tell the difference: Neurodivergent mood fluctuations are more likely to be situational and caused by external causes (rejection sensitivity dysphoria, related to work or school struggles related to ADHD, or sensory-based). Bipolar mood fluctuations are more likely to appear to have no cause (random and cyclical). It will be more difficult for the person to pinpoint a cause for the low mood as it is more biologically based. Furthermore, the mood shifts that occur in the context of BD tend to be longer than the mood shifts in ADHD. They also tend to be more cyclical and chronic and can be triggered more easily (Rodden and Olivardia, 2021)
What to look for (clinician): Does the person has a history of experiencing a depressed mood without cause? Does it have a cyclical nature to it? Also, be aware that a person with bipolar can have mixed (symptoms of both mania and depression) episodes.
Impulsivity/Risk Behavior
A hallmark of mania is risk-taking behavior (risky sexual behavior, driving fast, gambling, excessive spending, and more). While impulsivity with ADHD can also show up as reckless behavior, it is more likely to be due to not thinking through the consequences of their actions. In mania, a person may behave in ways that are farther from their values baseline.
What to look for (clinicians): What is the gap between the person’s values/baseline and the behavior? In the context of ADHD, reckless behavior is often due to difficulty thinking through the consequences of actions. In the context of mania, there is a disregard for consequences.
Stimming/Excessive Energy/Hyperactivity
Some of the characteristic experiences of mania can look like ADHD. For example, restlessness, talkativeness, distractibility, and fidgeting can be common both in the context of ADHD hyperactivity and in the context of mania.
What to look for (clinicians): in the context of Bipolar, this will be cyclical and will track with other symptoms of mania and will be absent in the context of depression. For the ADHD person, this will be a part of their baseline. Quality of energy: With ADHD, people can feel excited and energetic; manic energy, however, feels scary, uncontrolled, and uncontained (Rodden and Olivardia, 2021).
This can be difficult to tease out if the person has both ADHD and bipolar. In these situations, a person’s ADHD symptoms will become more exaggerated in the context of mania, and the person likely will benefit from both a stimulant (or bupropion) and a mood stabilizer to help with symptoms (Marks, 2019).
Starting Multiple Projects
Due to interest-based nervous systems and inattention difficulties, it is common in the context of ADHD to start multiple projects and fizzle out before they are completed. This is also common in the context of mania.
How to tell the difference: Assess whether this is happening in the context of other mania symptoms and is cyclical vs. a part of a person’s baseline experience. With ADHD, a person may be excited to start new projects but lose interest quickly. With mania, the person is frantically starting multiple projects and may struggle to complete projects, particularly if their mood shifts from mania to depression at which point they lose pleasure/interest in everything (Rodden and Olivardia, 2021). In the context of ADHD, the interest simply shifts to a new object.
Executive Functioning (Cognitive and Attention Difficulties)
This is a core feature of ADHD. In the context of ADHD, and the interest-based nervous system, when an activity isn’t innately interesting, focus and attention can become quite difficult. In the context of bipolar depression, the person can feel slow, unmotivated, foggy, and fatigued, which will contribute to attention problems and difficulty initiating new tasks.
Executive functioning difficulties are more dominant during a depressive episode in bipolar. However, research shows that these tasks continue to be difficult outside of a mood episode (Stern, 2017). Emerging research suggests that even outside of a mood disorder, people with bipolar continue to struggle with executive functioning tasks such as difficulty regulating attention, memory, and set-shifting (task-switching). As Stern notes:
Patients with bipolar disorder often manifest cognitive disturbances during acute manic, depressive, and mixed states, which include difficulties with attention, concentration, planning, and memory. It may come as a surprise, though, to learn that cognitive deficits can persist into euthymia – a state of relative mood stability. Indeed, approximately 40 % of euthymic bipolar patients show evidence of cognitive impairment involving attention, executive function (i.e., planning and organization, cognitive flexibility and set-shifting, and working memory), verbal memory, processing speed, and visual memory. Patients with bipolar I and bipolar II disorder appear to have a similar pattern of deficits.
Sleep Pattern Disruptions
It is common to have changes in sleep patterns in the context of ADHD. An estimated 25-50% of people with ADHD have sleep problems such as insomnia or other sleep disorder (such as circadian rhythm sleep disorder, sleep-disordered breathing, restless leg syndrome, and narcolepsy) Wajszilber et al., 2018. In the context of mania, a person’s sleep is often disrupted, and they may go with no to little sleep.
How to tell the difference: A key feature of mania is sudden sleep changes. A person may go from a fairly typical sleep schedule to sleeping only 1-3 hours a night and not feeling fatigued (or maybe awake for a few days straight). In the context of mania, the person will not be tired. In the context of ADHD, they will feel the impact of reduced sleep (executive functioning will often become worsened, and they will feel fatigued.)
Changes in Appetite
It is not uncommon for appetite and weight to ebb and flows in the context of ADHD. Appetite shifts are also common in the context of Bipolar. A person may lose their appetite and lose significant weight over a short period of time when in mania. On the flip side, the appetite may increase (or decrease) during a manic depression which will also contribute to weight fluctuation.
How to tell the difference: Assess to see if appetite weight change is connected to the underlying mood cycle (distinct manic symptoms or depressive symptoms) or if it is connected to behavioral/environmental factors. For example, if an ADHDer is hyper-fixated and hyper-focused on a project and thus eating less, their appetite changes are more situational.
Dissociation
Dissociation can have a wide range (from mild zoning out to identity shifts). Dissociation identity disorder can co-occur within bipolar at higher rates and may share some “neurophysiological architecture” Savitz et al., 2004. Dissociative experiences are common in the context of bipolar and are more common during a depressive episode (Chatterjee et al., 2018). Dissociation can also be linked to sensory overload. In sensory meltdown (the Fight-or-flight part of the nervous system), a person may respond with a more freeze effect to sensory overload, which can lead to mild forms of dissociation. Hargis, 2020
How to tell the difference: Assess whether this is occurring in the context of a mood disorder or triggered by sensory sensitivities. However, note that people with bipolar can also have sensory sensitives, although these tend to be more pronounced during a manic episode (while dissociation with bipolar tends to be more pronounced within a depressive episode).
Sensory Sensitivities
Speaking of dissociation. Let’s talk about sensory overload. Sensory sensitivity is a key feature of ADHD; it is a lesser-known aspect of bipolar. Recent research found that people with bipolar disorders were more sensitive to noise and other senses, which are correlated to differences in the brain and how it processes sensory information. It was found to be more common during mania (Wang et al., 2014)
Rejection Sensitivity
Rejection sensitivity dysphoria (intense reaction to perceived rejection) often co-occurs with ADHD. People with bipolar have also been shown to be more sensitive to rejection, which becomes heightened during a depressive episode (Ehnvall et al., 2014).
Hyper-Focus
People with ADHD do not have innate focus difficulties; they have difficulties regulating focus and can hyper-focus on a project of interest. During the context of mania, a person may also experience hyper-focus.
Loss of Pleasure vs. Boredom
It is common in the context of ADHD and mania to start many different projects and not finish them. In the context of ADHD, this may be associated with getting bored with projects easily. In the context of bipolar, the person may lose a sense of pleasure in all activities when in a depressive episode.
Shared Psycho-Social Risks
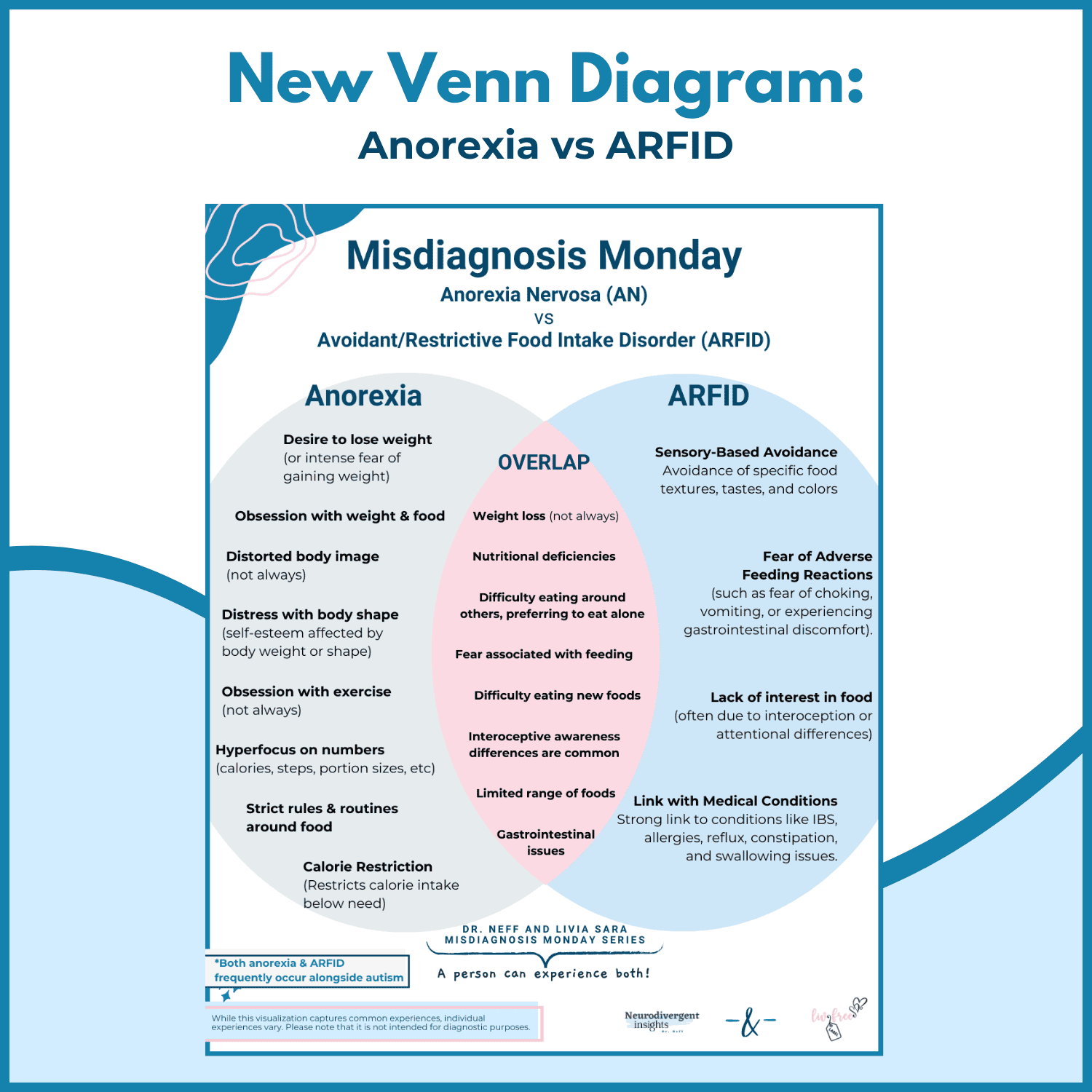
Co-occurring Eating Disorders
Co-occurring eating disorders are common in both.
Research has found that many people with bipolar disorder have eating issues like bulimia nervosa, anorexia nervosa, and binge-eating disorder. A recent study found 14% (approximately 1 in 7) of people with bipolar met the criteria for a lifetime eating disorder (McElroy et al., 2011).
Biederman et al., 2007 found that ADHD girls were 3.6 more likely to have an eating disorder. ADHD girls were 5.6 times more likely to have bulimia than the general population Biederman et al., 2007. Similarly, Bleck et al., 2015 found ADHD had a significantly higher rate of eating disorders (4.2%) than the non-ADHD population (2.0%) and had 2.8 times more likely to have an eating disorder.
Addiction
Addiction is common among both ADHDers and people with Bipolar. This may be related to a tendency to self-medicate, self-soothe, regulate sensory experiences, or may occur in the context of co-occurring depression/anxiety.
Several studies have shown a correlation between ADHD, drug abuse, and alcoholism. ADHD is estimated to be 5 to 10 times more common among adult alcoholics. Among adults being treated for alcohol and substance abuse, the rate of ADHD is about 25% (WebMD)
Smith et al., 2002 found that approximately 25% of adults and 30% of adolescents receiving treatment for alcoholic disorder have ADHD (for reference, approximately 2-5 % of adults and 3-7 % of children have ADHD).
Estimates of co-occurring substance abuse disorder in the context of Bipolar range from 41- 60% for Bipolar I and a 20% prevalence rate for bipolar type II (Cerullo et al., 2007). Drugs and alcohol often make symptoms of bipolar worse. One study found alcohol was the most commonly abused drug (Chengappa et al., 2000).
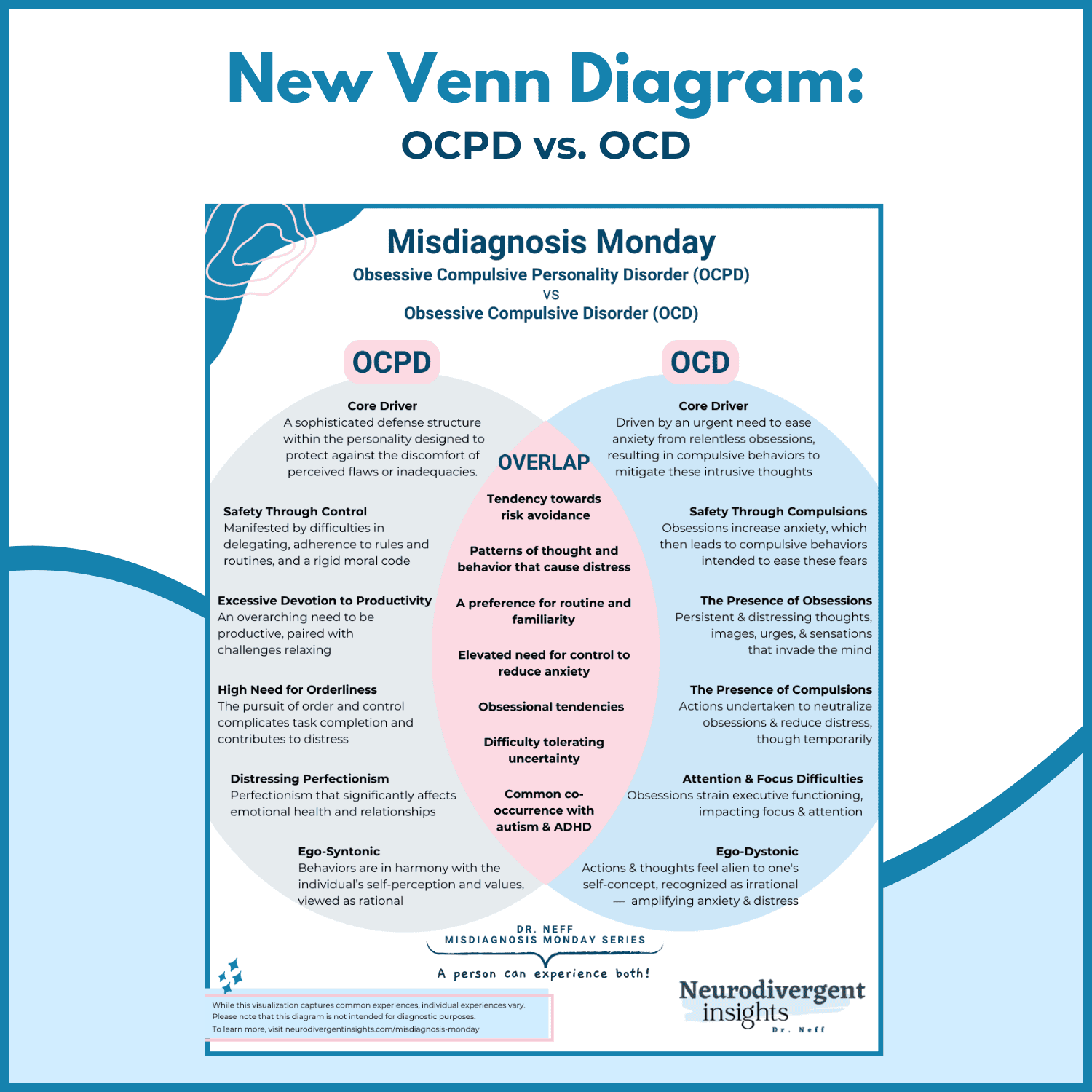
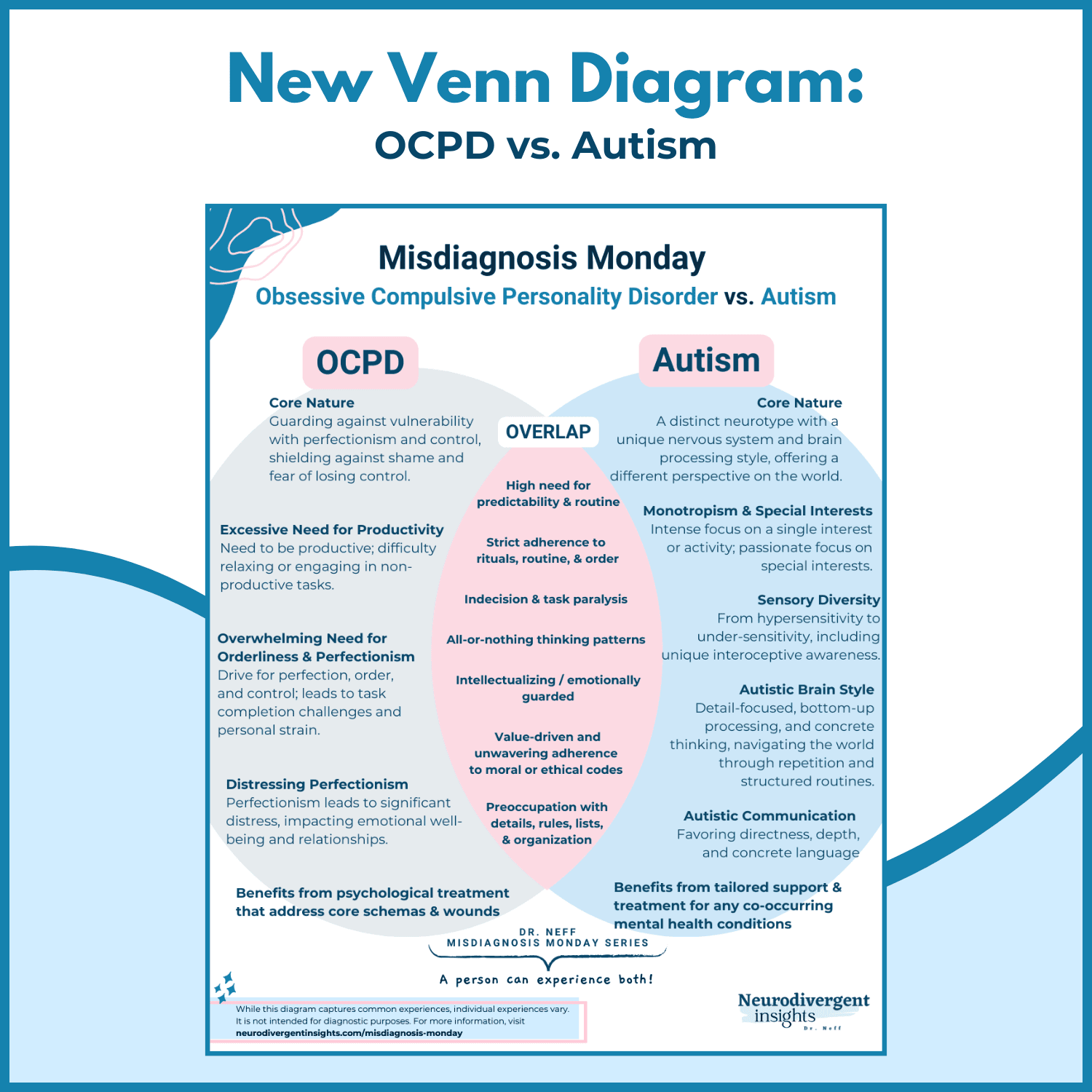
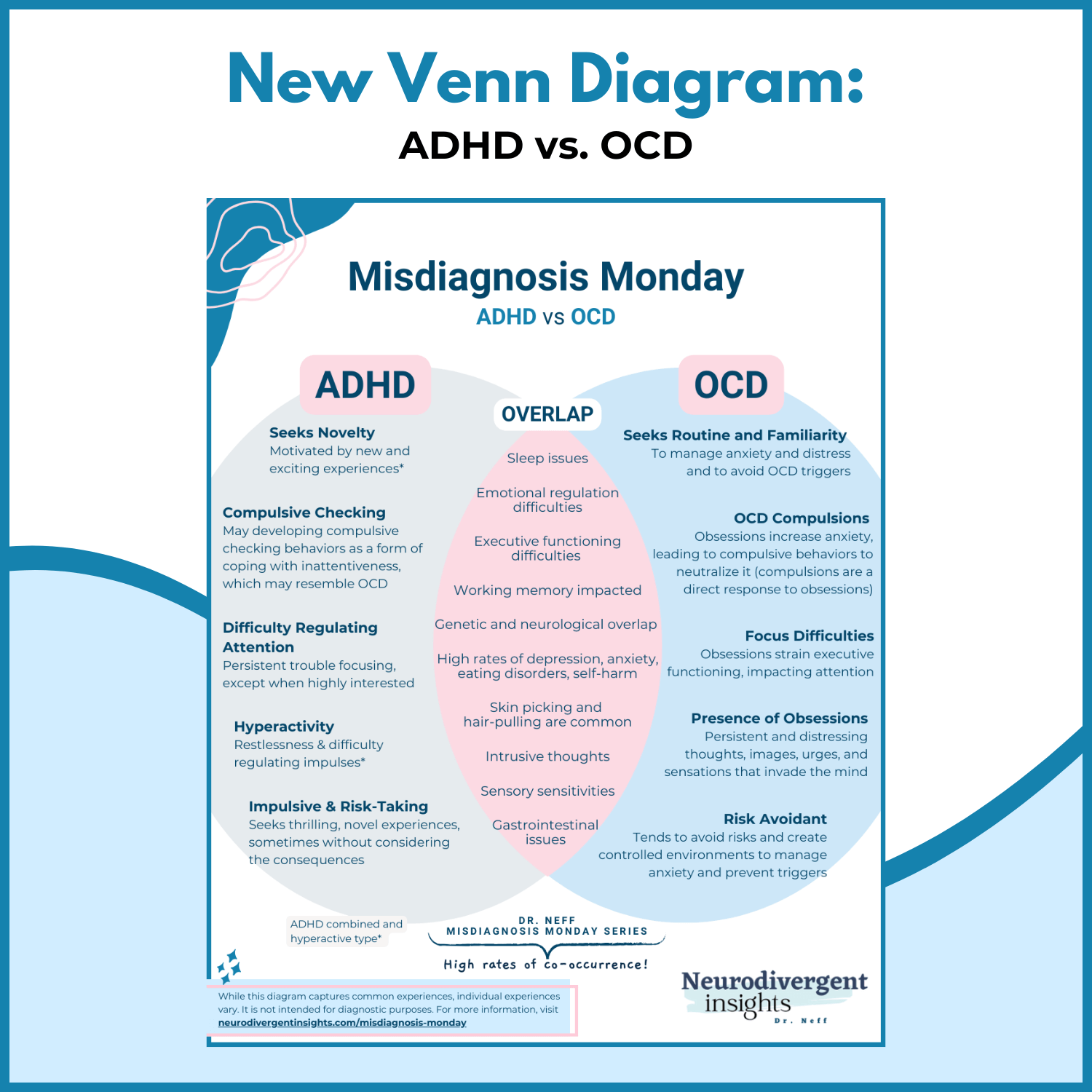
OCD
Both have significantly higher rates of OCD, and similar neural circuitry is involved in all three conditions.
The prevalence rate for OCD among ADHDers is estimated to be around 30% (Geller et al., 2002). And 25% of people with OCD are estimated to have ADHD (Walitza et al., 2008).
The Lifetime co-occurrence of OCD among people with bipolar was 11–21% in BD patients. A co-occurrence of Bipolar occurred in 6–10% of OCD patients. Compared to purely OCD patience, BD-OCD was characterized by more Obsessive-Compulsive (OC) symptoms. (OC symptoms increased during the depression and improved during mania/hypomania. BD-OCD patience also tended to have more depressive episodes and more antidepressant-induced mania/hypomania experiences (Amerio et al., 2014). People with BD-OCD also had increased risks associated with suicidality and substance abuse than BD people without co-occurring OCD Amerio et al., 2014).
Self-Harm and Suicidality
Self-harm behavior and suicidality are high among both groups. Self-harm may occur as an attempt to regulate sensory load or may be used as an attempt to regulate difficult emotions.
Self-harm is alarmingly high among girls with ADHD. Girls are more prone to internalize many ADHD symptoms. The risk of self-harm behavior is highest among those with ADHD combined type Allely, 2014; Hinshaw et al., 2012 found that self-harm behavior happened at a rate of 69% among adolescents with ADHD (compared to 32% non-ADHDers). Self-harm has also been noted to be more common among Autistic girls and Autistic-Trans/gender-diverse (Dudas et al., 2017)
Previous research has consistently shown a connection between ADHD and suicidal ideation and behaviors. The correlation was strong for both men and women (Allely, 2014). Hurtig et al., 2012 evaluated the relationship between ADHD and suicidal and self-harm behavior among adolescents. They found that when compared to non-ADHD adolescents, ADHD adolescents experience more suicidal ideation (57% compared to 28%).
The rate of suicidality is approximately 10-30 times higher among people with bipolar and approximately 20% of people with bipolar (mostly untreated) die by suicide, and 20-60% of people with bipolar have had at least one suicide attempt during their lifetime (Dome et al., 2019).
A recent study found elevated rates of self-harm among people with bipolar over people with depression (52% versus 37%, respectively)… Approximately 37% of bipolar youth engaged in self-harm, and 52% of adults with bipolar had at least one episode of self-harm (compared to 37% with depression) (Weintraub et al., 2017).
Victimization
Both groups have elevated rates of peer victimization. This happens at even higher rates for people with ADHD or Bipolar who have other marginalized identities.
ADHD: ADHD traits, particularly hyperactivity-impulsivity, are correlated with an increased risk of peer victimization (Papadopoulos et al., 2021). Humphrey et al., 2007 also found a correlation between peer victimization and ADHD.
Rates of victimization were found to be exceptionally high among girls with ADHD (Wiener and Mak, 2009).
One study found that 1 in 3 people with bipolar was victimized. Females were twice as likely to be victimized compared to males (White et al., 2006).
How to Spot the Difference
Screening for ADHD
Screening questions from Katzman et al., 2017:
Have you had long-standing and consistent problems with attention and distractibility?
Have your current complaints been present over the last 10 or 20 years?
If I could see you in the classroom when you were a child, what would you be like?
If the above screening questions indicate the possible presence of ADHD, a routine screener such as the Adult ADHD Self-Report Scale (ASRS) can be used. Furthermore, an in-depth clinical interview for ADHD, such as the ACE+ (Free to download). You may also include
· Wender-Reimherr Adult Attention-Deficit Disorder Scale (WRAADDS),
· Conners Adult ADHD Rating Scales (CAARS)
· Barkley Deficits in Executive Functioning (BDEFS for Adults)
· Weiss Functional Impairment Rating Scale (WFIRS) (PDF)
· Adult ADHD Quality of Life Scale (AAQoL)
Bipolar Screener
Assess for Psychosis: In the context of Bipolar 1, a person may have psychotic symptoms (delusions or hallucinations. Such symptoms are more common in the context of mania. These are not symptoms of ADHD.
Assess for classic manic symptoms: an inflated sense of ego or grandiosity (that is different than baseline).
Routinely implement The Mood Disorder Screener into ADHD assessments/intake paperwork.
You may also consider including the DES-II, given that there is a higher rate of dissociative experiences in the context of bipolar. DES-II is a 28-item scale rated in the percentage of 0 to 100 with increments of 10, and it is designed to measure the frequency of dissociative experiences (designed for 18+)
Clinical Interview: For a list of screening questions, see the last several slides on this PowerPoint from UW PACC, “Bipolar disorder-Screening and diagnosing in Primary Care” or consider purchasing and using the SCID-5-CT
Considerations for Prescribers and Clinicians
Medication Considers
There are mixed reports regarding medication. While current research points to stimulation medication being safe in the context of bipolar and continuing to be used as first-line therapy in the treatment of ADHD/bipolar, there is some potential risk that stimulant therapy could exacerbate or induce mania (Katzman et al., 2017).
The person will likely benefit from closer medication management/monitoring to ensure stimulant does not exacerbate mania (Katzman et al., 2017). Prescribers who want to proceed with caution may choose to start with bupropion as first-line therapy for people with co-occurring ADHD/bipolar. For example, the Canadian Network for Mood and Anxiety Treatments (CANMAT) recommends bupropion as first-line therapy for individuals with comorbid ADHD and bipolar disorder, followed by a stimulant (Katzman et al., 2017).
Others have suggested that using a long-acting stimulant can be useful once the mood is stabilized with a mood stabilizer. However, the person should still be monitored closely regarding the potential for stimulant-associated mania/hypomania (Katzman et al., 2017).
Resources
For clinicians working with ADHD: Executive Functions by Russell Barkley or check out my book recommendations for Neurodivergent Clinicians (#affiliatelinks)
ADHD Reads: Outside the Box, Women with ADHD
Bipolar Reads: The Bipolar II Disorder Workbook and The Bipolar Disorder Survival Guide
***Bipolar Resource for Clients: https://www.cci.health.wa.gov.au/Resources/Looking-After-Yourself/Bipolar (Free, self-paced workbooks for bipolar-a wonderful resource on how to keep a balance, provides a place to record symptoms, and provides behavioral and cognitive strategies to help with managing moods).
Citations
Amerio A, Odone A, Liapis CC, Ghaemi SN. Diagnostic validity of comorbid bipolar disorder and obsessive-compulsive disorder: a systematic review. Acta Psychiatr Scand. 2014;129(5):343-358. doi:10.1111/acps.12250
Cerullo, M.A., Strakowski, S.M. The prevalence and significance of substance use disorders in bipolar type I and II disorder. Subst Abuse Treat Prev Policy 2, 29 (2007). https://doi.org/10.1186/1747-597X-2-29
Chatterjee, S. S., Pal, A., Mallik, N., Ghosal, M., & Saha, G. (2018). Dissociative Experience in Unipolar and Bipolar Depression: Exploring the Great Divide. Clinical psychopharmacology and neuroscience : the official scientific journal of the Korean College of Neuropsychopharmacology, 16(3), 262–266. https://doi.org/10.9758/cpn.2018.16.3.26
Chengappa, K. R., Levine, J., Gershon, S., & Kupfer, D. J. (2000). Lifetime prevalence of substance or alcohol abuse and dependence among subjects with bipolar I and II disorders in a voluntary registry. Bipolar Disorders, 2(3), 191-195. https://doi.org/10.1034/j.1399-5618.2000.020306.x
Dome, P., Rihmer, Z., & Gonda, X. (2019). Suicide Risk in Bipolar Disorder: A Brief Review. Medicina (Kaunas, Lithuania), 55(8), 403. https://doi.org/10.3390/medicina55080403
Ehnvall, A., Mitchell, P. B., Hadzi‐Pavlovic, D., Parker, G., Frankland, A., Loo, C., … & Perich, T. (2014). Rejection sensitivity and pain in bipolar versus unipolar depression. Bipolar disorders, 16(2), 190-198. https://doi.org/10.1111/bdi.12147
Hargis, B. (2020, January 1). Overstimulation and the Dissociative Brain, HealthyPlace. Retrieved on 2021, November 14 from https://www.healthyplace.com/blogs/dissociativeliving/2020/1/overstimulation-and-the-dissociative-brain
Katzman, M.A., Bilkey, T.S., Chokka, P.R. et al. Adult ADHD and comorbid disorders: clinical implications of a dimensional approach. BMC Psychiatry 17, 302 (2017). https://doi.org/10.1186/s12888-017-1463-3
Marks, Tracey. “ADHD Vs. Bipolar Disorder – How to Tell the Difference” YouTube Video. Retrieved at: https://www.youtube.com/watch?v=pGUvXPL57as&ab_channel=Dr.TraceyMarks
McElroy, S. L., Frye, M. A., Hellemann, G., Altshuler, L., Leverich, G. S., Suppes, T., … & Post, R. M. (2011). Prevalence and correlates of eating disorders in 875 patients with bipolar disorder. Journal of affective disorders, 128(3), 191-198. https://doi.org/10.1016/j.jad.2010.06.037
Parker, G., Paterson, A., Romano, M., & Graham, R. (2017). Altered sensory phenomena experienced in bipolar disorder. American Journal of Psychiatry, 174(12), 1146-1150. https://doi.org/10.1176/appi.ajp.2017.16121379
Savitz, J., Solms, M., Pietersen, E., Ramesar, R., & Flor-Henry, P. (2004). Dissociative identity disorder associated with mania and change in handedness. Cognitive and behavioral neurology : official journal of the Society for Behavioral and Cognitive Neurology, 17(4), 233–237.
Schiweck, C., Arteaga-Henriquez, G., Aichholzer, M., Thanarajah, S. E., Vargas-Cáceres, S., Matura, S., … & Reif, A. (2021). Comorbidity of ADHD and adult bipolar disorder: A systematic review and meta-analysis. Neuroscience & Biobehavioral Reviews. https://doi.org/10.1016/j.neubiorev.2021.01.017
Stern, Susan (2017). “‘My Mood is Better So why I struggline so Much?’: Cognitive Challenges in Bipolar Disorder”. Chicago Psychiatry Associates. Retrieved at: https://www.chicagopsychiatryassociates.org/blog/2017/11/13/my-mood-is-better-so-why-am-i-struggling-so-much-cognitive-challenges-in-bipolar-disorder/
Wajszilber, D., Santiseban, J. A., & Gruber, R. (2018). Sleep disorders in patients with ADHD: impact and management challenges. Nature and science of sleep, 10, 453–480.https://doi.org/10.2147/NSS.S163074
Wang, Y., Feng, Y., Jia, Y., Wang, W., Xie, Y., Guan, Y., … & Huang, L. (2014). Auditory M50 and M100 sensory gating deficits in bipolar disorder: A MEG study. Journal of affective disorders, 152, 131-138. https://doi.org/10.1016/j.jad.2013.08.010
Weintraub, M. J., Van de Loo, M. M., Gitlin, M. J., & Miklowitz, D. J. (2017). Self-Harm, Affective Traits, and Psychosocial Functioning in Adults With Depressive and Bipolar Disorders. The Journal of nervous and mental disease, 205(11), 896–899. https://doi.org/10.1097/NMD.0000000000000744
White, M. C., Chafetz, L., Collins-Bride, G., & Nickens, J. (2006). History of arrest, incarceration and victimization in community-based severely mentally ill. Journal of community health, 31(2), 123–135. https://doi.org/10.1007/s10900-005-9005-1