Bipolar and Autism
I started this series with a desire to help distinguish Autism from common misdiagnoses. While that is still one of my goals, the deeper I tread into the literature, I realize it is so much more complex than this. While it’s challenging to get accurate statistics, Autism frequently co-occurs with at least one other mental health/health condition (PsychiatryAdvisor). Bipolar is one of the conditions that co-occur with Autism at higher rates (than compared to the general population).
Recent studies suggest Autism and Bipolar share genetic links and can commonly co-occur in families. Other studies have demonstrated genetic links between schizophrenia, bipolar, and autism and identified that they share similar genetic expression patterns in the brain (Zeliadt, 2018). They all activate certain genes in the astrocytes–star-shaped brain cells that perform key functions in the central nervous system Gandal et al., 2018.
Similarly, all three conditions suppress genes that help synapses (the connection point between nerve cells in the brain). So neurologically they have similarities (and thus there are many overlapping traits of the conditions), and genetically they are connected meaning there likely co-occur at higher rates. Given this, it can be difficult to discern what is an overlap of bipolar and autistic traits in a person, and what is true co-occurrence. Here are some prevalence rates from recent studies:
30% of youth 7-17 with bipolar also met the criteria for Autism (Joshi et al., 2013).
47.2% of adults with bipolar showed a clinically significant level of Autistic Traits (Abu-Akel et.al, 2017).
27% of children w/ pervasive developmental disorder also had bipolar (Raja & Azzoni, 2008) (compared to 4% of the general population).
The high level of trait overlap increases the likelihood of misdiagnosis; thus, it is difficult to know the true prevalence of Autism and bipolar co-occurrence. However, given the genetic link between the two conditions, co-occurrence is more common than among the general population. Thus, making it particularly murky waters to wade through. Before highlighting the overlapping characters and traits, let me first offer a brief overview of bipolar.
Contents:
Bipolar 101
Bipolar, like Autism, is considered a form of neurodivergence. It is characterized by distinct mood swings between mania and depression. Moods may cycle quite rapidly or be more prolonged and distinct from one another. Some mood episodes will have “mixed features” where they experience both elements of “highs” and “lows” within a single episode or have rapid cycles of highs/lows. Hallucinations may be present during mania. Approximately 2.8-4.4% of the U.S population has some form of bipolar within their lifetime (NIH)
Symptoms of Bipolar Disorder Include
Distinct manic episodes
Hypomanic episodes (similar to mania but generally shorter episodes and can feel more manageable)
Depressive episodes
Mixed episodes (both symptoms of mania and depression are present at the same time or in rapid succession)
Psychotic symptoms (typically during mania, not everyone experiences this)
Symptoms Associated with Mania
More energized than usual despite a reduced desire and ability to sleep
Feeling so hyper that person doesn’t act like their usual self
Experiencing rapid shifting ideas, uncontrollable racing thoughts, or quickly changing topics when speaking
Excessive talking/speaking faster than typically
More social and outgoing than typical
Increased self-confidence and grandiosity (feeling invincible or on top of the world)
An increase in activity levels, engagement, or restlessness. The person may work on multiple projects simultaneously
An increase in irritability and aggression may be present
Pressured speech (increased or faster than usual)
Engaging in risky behaviors (risky driving, sexual practices, substances, or spending)
Increased impulsivity (related to spending, sex, substances)
Hallucinations (less common)
Symptoms Associated with Bipolar Depression Include:
Reduced or lost interest in activities previously enjoyed
Unexplained fatigue and exhaustion
Feeling intense, overwhelmingly sadness, hopeless, and worthlessness
Changes to sleep and appetite
Difficulty concentrating and focusing
Thoughts of suicide and death
If you need a refresher on autism, go check out my post, social anxiety vs. autism, where I review the DSM criteria of Autism. Following are some of the overlapping characteristics/traits that make it difficult to distinguish between the two:
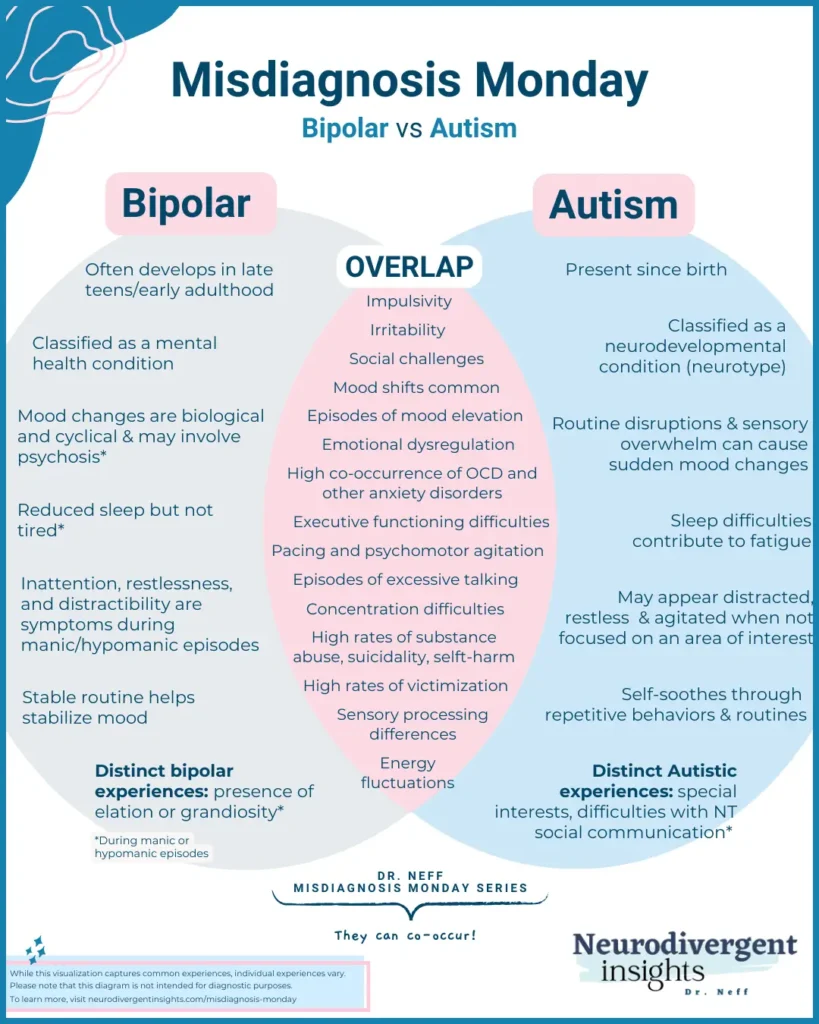
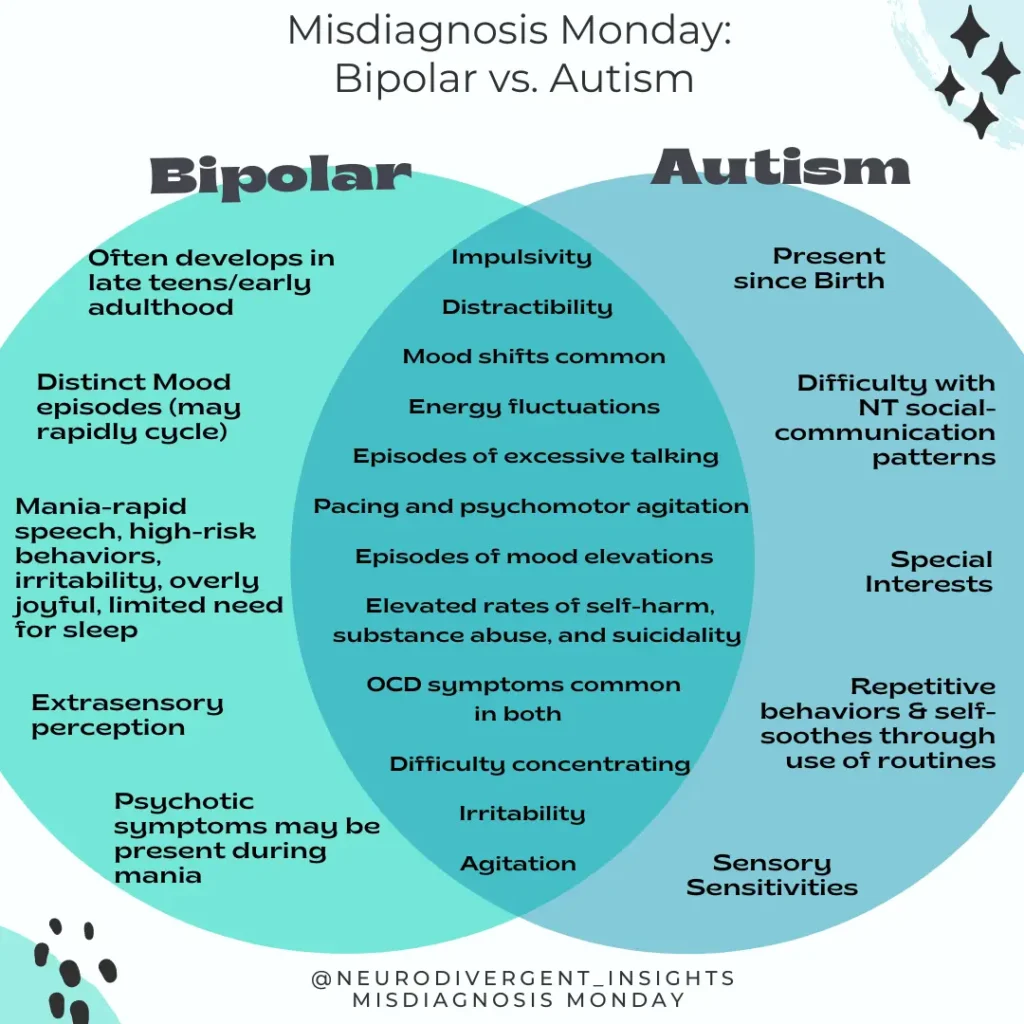
Overlapping Characteristics and Traits
Overlapping Characteristics
Neurodivergent energy flux and quick emotional shifts (tendency to experience emotions in extremes) can look like the ebb and flow of mania/depression.
Elevated or depressed mood: Elevated mood in Autism may be related to special interest energy, and depressed mood may be related to burnout or co-occurring depression
Special interest energy can be directed toward people (infatuation/obsessions, this can also look like manic energy)
Intense irritability/Aggression: Often present during mania, can be associated with sensory sensitivities/meltdown
Excessive talking: Present in mania also can be present with special interest “info-dumping”, talking can also be a form of a repetitive behavior
Distractibility: Related to mania/depression and related to executive difficulties in the context of Autism
A tendency to “get in trouble” or do risky things”: A feature of mania can be related to impulsivity/executive function in the context of Autism (particularly among children and youth)
Repetitive activities or behaviors, such as pacing: Can be related to excess energy in mania or stimming behavior in the context of Autism
Sleep disturbances: Mania or Autism sleep profile (the Autist without bipolar will more likely to be disturbed/impacted/fatigued by loss of sleep)
Being accident-prone: Mania impulsivity or autistic visual-motor difficulties
Racing thoughts or trouble organizing thoughts: Present in Mania or can be related to a flood of thoughts in the context of special interest energy or neurodivergent communication patterns
OCD Symptoms common in both groups
Overlapping Traits
Witwer and Lecavalier, 2010 found that symptoms associated with “mania” in Autistic children aged 7-17 were manifestations of their autistic traits. Some autistic traits reported in a study of autists children (7-17) that look like mania included:
Frequent episodes of elevated mood (30%)
Presenting as “Very irritable” (60%)
Excessive Talking (50%)
Pacing and excessive activity (43%)
Accident proneness (44%)
Distractibility (43%)
Tendency to get in trouble (43%)
Sleep disturbances
Overlapping Psycho-Social Risks
In addition to overlap in trait/symptom expression, we share many shared psycho-social risks–from substance abuse to victimization to the risk of dying by suicidality.
Higher Risk of Suicidality
People with bipolar are 10 to 30 times more likely to die by suicide than people without bipolar (people are most at risk during a mixed episode) (Fries, 2020). Approximately 20% of people with bipolar (mostly untreated) die by suicide (Dome, et al., 2019). And 20-60% of people with bipolar attempt suicide at least once in their lifetime (Fries, 2020).
A recent longitudinal study involving 6.5 million people found that Autists were three times more likely to both attempt suicide and to die by suicide. Women on the spectrum are at a higher risk than both men on the spectrum and neurotypical females. This is notable, given that within the general population, the risk of death by suicide is higher for men (Bhandari, 2020). Suicidality was particularly high among youth and young adults. Suicidality was also more elevated for those with a co-occurring mood disorder such as anxiety or depression (South et al.)
Higher Rates of Substance Abuse
The presence of substance abuse disorder among people with bipolar is at least 40%, but some studies have found as many as 60% of the population (Cerullo, 2007).
A recent study in Sweden found that Autists with average to high intelligent quotients (IQ) were twice as likely to struggle with addiction to alcohol or other drugs. Among Autists, drugs are sometimes used to cope with social stress and sensory problems (Szalavitz).
Higher Rates of Victimization
People with bipolar, particularly women, have higher rates of victimization (28% in Darves-Bornoz study, 1995); other studies have put victimization rates as high as 1/3 of people with bipolar.
Recent research has demonstrated that Autist women are more likely to be survivors of violent victimization. Some risk factors include the challenge in social reasoning, missing contextual cues, and a tendency to take things literally. In one study, Autistic adults were 7.3 times more likely to endorse having experienced sexual assault from a peer during adolescence (Weiss and Fardella).
Both groups have an Elevated Risk of Self-Harm Behavior
While many clinicians continue to associate self-harm with Borderline Personality Disorder, it is also common among people with Bipolar and Autism.
Joyce et al., 2010 study found a particularly strong association between bipolar and self-harm.
Self-harm is also common among Autists; it can be a way for the Autist to self-soothe or ground following sensory overload and emotional dysregulation. One study found that parents reported self-harm behavior among their autistic youth in 15% of cases (Huang).
The Importance of Diagnosing Co-Occurring Autism/Bipolar
For several reasons, it is vital to understand when these conditions co-occur. The psycho-social risks highlighted above are likely exacerbated when both conditions are present. The co-occurrence also has important implications for medications:
Many Autists have co-occurring mood disorders and OCD symptoms and thus might seek medication such as an anti-depressant (SSRI). However, for many people with Bipolar, an SSRI can make symptoms of mania worse. It is typically recommended to avoid SSRIs in the context of Bipolar (or to have close monitoring when starting an SSRI) (Raja & Azzoni, 2008). If a person is diagnosed with Autism, but their Bipolar remains undiagnosed, a prescriber may start them on an SSRI without recognition of the associated risk.
Lithium, widely used to treat Bipolar, can be a highly toxic medication. Autists bodies can be more sensitive to mediations and toxins and, therefore may have more extreme reactions. When a person is put on lithium, it is vital they communicate with their loved ones and doctors about their experiences with the medication. If an Autist struggles with interoception (difficulty observing body signals) or has communication differences/difficulties and is unable to communicate about the medication’s troublesome side effects, this can be dangerous. Some studies have suggested that starting with anti-seizure medication, and mood-stabilizing medications with low-dose of anti-psychic medication are safer for Autists. If Bipolar is diagnosed, but the Autism remains undetected, such precautions around toxicity, side effects and medicine may be disregarded (National Autistic Society UK).
Clinician’s Corner: How to Spot the Difference
Traditional methods of assessing for bipolar (and other psychiatric disorders) may not be appropriate for autists; therefore, someone familiar with Autism should provide the assessment when possible. On the flip side, many clinicians who are comfortable assessing Bipolar are unfamiliar or uncomfortable assessing autism; therefore, autism may not be on their radar (differential list) when assessing for bipolar. Therefore, it is likely many people have been diagnosed with Bipolar while their Autism goes undetected, and some Autists have likely been diagnosed with autism while their Bipolar remains undetected. And there are likely Autists who aren’t Bipolar and have been misdiagnosed as Bipolar. Goodness, this gets confusing! It is less likely that allistics who are bipolar are misdiagnosed as Autistic.
If you are a clinician who regularly diagnoses bipolar, you should familiarize yourself with autism and have it on your differential list (given the high genetic overlap between the two conditions). And vice versa; if you are a clinician who regularly assesses for Autism, you should familiarize yourself with Bipolar.
In Discerning if it is Bipolar (vs. Autism)
It is important to distinguish if the symptoms of mania have been present together for a distinct duration of time. And has it contributed to significant problems for the person (i.e., spending their life’s saving impulsivity, engaging in unsafe sex practices they typically wouldn’t, behaving in ways that aren’t consistent with their underlying values, etc.)? Tease out whether there are distinct cycles to symptoms of mania/depression. The Mood Questionnaire is a solid routine screener to use for capturing whether these symptoms appear together and would be a beneficial screener to include in your Autism battery. You may also consider having the client track mood in a mood tracker for 1-3 months.
Work to tease out the underlying motivation/origin of trait expression. For example, work to tease out if excessive talking is part of an overall manic presentation or dependent on special interest energy. Is excessive pacing part of the person’s baseline behavior and an aspect of stimming behavior consistent with Autism, or is it a new expression in the context of other manic symptoms?
Review the medical history-has the person ever been on an SSRI? Did it make mood symptoms worse? Family history of bipolar or Autism?
Consider the age of onset of mood symptoms. Autist Youth with bipolar tends to show mood symptoms earlier than allistics with bipolar.
If Discerning if the Bipolar Client is also Autistic
Assess for the presence of Criteria A (difficulty with social communication, intuitively interpreting others)
Assess for the presence of Criteria B: look for repetitive behaviors, special interests, rituals, and sensory issues.
Assess for alexithymia, interoception, differences in social motivation, executive functioning difficulties, processing speed, auditory processing disorder, and other conditions that commonly present alongside Autism.
If possible, interview a family member to see if symptoms were present in infancy/early childhood.
Consider the presentation of bipolar symptoms. Symptoms of bipolar in the autist can be different than when manifested in a neurotypical. For example, youth with both tend to show an earlier age of onset of mood symptoms (than youth with just BP) (Borue et al., 2016). Some common mania symptoms for people who have both Bipolar and ASD include:
Pressured speech (rapid, loud, incessant)
Constant pacing
Easily distractibility and risky behavior
Goal-directed agitation and irritability were symptoms of mania in all ASD+BD participants
92.5% showed increased risky behavior and distractibility during mania
90% showed decreased sleep during mania
82.5% showed over-talkativeness,
Increased stereotypic behavior (62.5% of cases)
Obsessions are more common (present in 60% of cases)
A sudden decrease in sleep
More Socially withdrawn
Morel likely to have a depressed mood
A sudden increase in impulsivity and aggression
More difficulty in friendships
Source (Sapmaz et al., 2018 and Borue et al., 2016)
If you suspect both, the client will likely benefit from pharmaceutical support. Consider close monitoring of any medication used to support the client. Given the need to attend to toxic load (for the Autist), and the need to attend to risk of mania (for the Bipolar client), it is imperative to have close monitoring when initiating medication for the person who presents with clusterings of Autistic/Bipolar traits.
Follow Up Resources
Bipolar Workbook (Free): Developed by Australian Psychologists, this is a great self-paced workbook for managing bipolar symptoms.
Autism Screeners
AQ: Autism Spectrum Quotient
Aspie Quiz (can download PDF of results). You need to create a login account in order to get results. Will show both neurotypical and neurodiverse traits
The Ritvo Autism Asperger Diagnostic Scale-Revised (RAADS-R) is a self-report questionnaire designed to identify adult autistics who “escape diagnosis” due to a subclinical level presentation.
EQSQ: Combined version of Baron-Cohen’s Empathizing Quotient (EQ) and Systemizing Quotient (SQ)
The Camouflaging Autistic Traits Questionnaire (CAT-Q) is a self-report measure of social camouflaging behaviors in adults. It may be used to identify autistic individuals who do not currently meet diagnostic criteria due to their ability to mask their autistic proclivities.
The Big 5 Personality Assessment (Not a test for Autism, but certain patterns are often consistent with Autism).
Bipolar Screener
https://www.sadag.org/images/pdf/mdq.pdf