Dorsal Vagal Shutdown: How to Identify a Shutdown
Affiliate Disclaimer: This article contains affiliate links, which means receive a commission if you click a link and purchase something that we have recommended. Please note that clicking these links won’t cost you any extra money, but they help us keep this site up and running. Thank you for your support!
Do you ever find yourself battling chronic fatigue, persistent depression, migraines, or a sense of disconnection from life? If so, you're not alone. These symptoms can stem from various sources, but one lesser-known culprit might be lurking beneath the surface: Dorsal Vagal Shutdown.
You may be wondering, "What exactly is that?" Despite its significance, the term remains unfamiliar to many. While the concept of "freezing" in response to crisis is widely recognized, there's less awareness about the prolonged states of withdrawal and disconnection attributed to Dorsal Vagal Shutdown.
This experience is marked by dorsal vagal dominance, triggering a significant withdrawal from interaction with the external world. It can also emerge from sensory overload, leading to a sensory shutdown—making this an important topic for neurodivergent individuals to understand.
In this article, we'll explore Dorsal Vagal Shutdown, including its mechanisms, differences between acute and chronic shutdown, and shed light on how to identify a shutdown and how to support it.
What is Dorsal Vagal Shutdown?
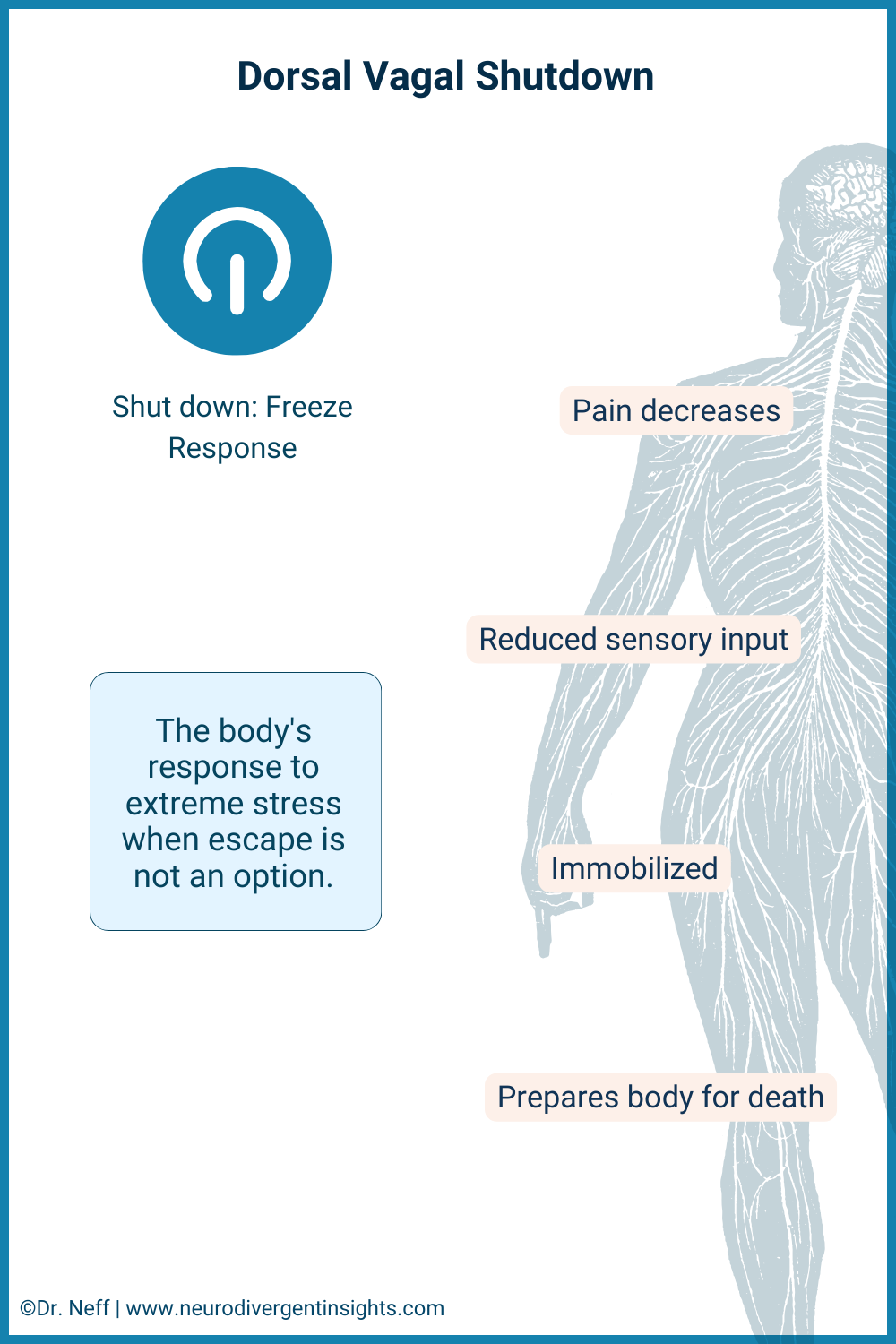
Dorsal Vagal Shutdown is like our body's natural response to hitting the pause button when faced with extreme stress or trauma. It's a state where everything slows down internally to conserve energy, akin to dimming the lights and volume around us for some quiet. This response, managed by the dorsal branch of the vagus nerve, triggers what's known as a "freeze" state.
In this mode, the body prioritizes protection, significantly reducing pain signals and lowering both mobility and arousal levels—as if preparing for a situation it cannot escape from, almost like preparing for death. This might result in our feeling extremely tired, numb, or disconnected from both the world around us and from our own emotions. It's the body's way of shielding itself during overwhelming situations.
Especially for people who are neurodivergent, like those who are Autistic, Dorsal Vagal Shutdown is a key concept for understanding our distinct responses to stress. Emerging research indicates that, compared to non-autistic individuals, we are more likely to experience a shutdown response to stress rather than the fight-or-flight reaction. This can manifest as an outward appearance of calmness, masking significant internal disconnection and immobility. Recognizing this distinction is important, as it sheds light on the profound, though often invisible, ways stress impacts neurodivergent people.To delve deeper into the nuances of the neurodivergent nervous system and its responses, you can read more here.
The Parasympathetic Nervous System
Understanding Dorsal Vagal Shutdown deepens with an exploration of the Parasympathetic Nervous System's (PNS) role. As a crucial branch of the Autonomic Nervous System, the PNS is responsible for our "rest and digest" functions, providing a counterbalance to the Sympathetic Nervous System's (SNS) "fight-or-flight" responses.
The PNS initiates a shutdown response when under overwhelming stress, conserving energy through mechanisms like fatigue, dissociation, and, occasionally, blackouts. This response holds particular significance for Autistic individuals, where variations in sensory processing and emotional regulation can intensify shutdown states, leading to what appears as calmness but masks deep internal disconnection.
The Vagus Nerve
The vagus nerve, stretching from the brainstem down to the abdomen and influencing the heart, lungs, and digestive system, plays a pivotal role in our body's autonomic functions. It acts as a critical communication link, overseeing vital processes from speech to heartbeat regulation and digestion.
Central to the PNS, the vagus nerve helps us return to a state of calm following moments of stress or danger. Polyvagal Theory introduces us to the dual nature of this nerve: one branch fosters social connectivity and tranquility; while the other triggers a protective "freeze" response in the face of severe stress, similar to how an animal will “play dead” in the wild as a survival strategy.
Excessive stress can lead to an overreaction of this freeze mechanism, resulting in a state of immobilization or numbness. This response, while a defense mechanism, can significantly impact mental health and stress management, particularly for neurodivergent individuals who may experience these states more acutely or frequently due to our unique neurological wiring.
Vagal Tone
A closely related concept is vagal tone. While vagal tone might not be a household term, it holds significant sway over our health and emotional well-being. Vagal tone, a crucial measure of the health and flexibility of the vagus nerve, significantly impacts our overall well-being. High vagal tone is associated with better emotional and physical health, including lower blood pressure and improved immune function.
Conversely, lower vagal tone may increase susceptibility to physical health conditions, stress and anxiety, and affect recovery from physical or emotional challenges.
Enhancing vagal tone through practices such as mindful breathing, laughter, engaging in joyous and creative activities, and engaging in pleasurable movement can support better stress management and resilience, especially beneficial for Autistic and ADHD people who more often experience reduced vagal tone and flexibility. You can also use vagal nerve stimulators such as the sensate, safe and sound protocol, or a Tens unit with ear clips.
Interested in learning more about how vagal tone is assessed? You can read more about the link between heart rate variability and vagal tone here.
Hypoarousal or Dorsal Vagal Shutdown?
Let's look at another concept connected to all this: hypoarousal. Imagine our nervous system like a car's engine that can run at different speeds. Ideally, the engine runs smoothly, balancing acceleration (sympathetic branch) and slowing down (parasympathetic branch) to respond well to whatever road we’re on.
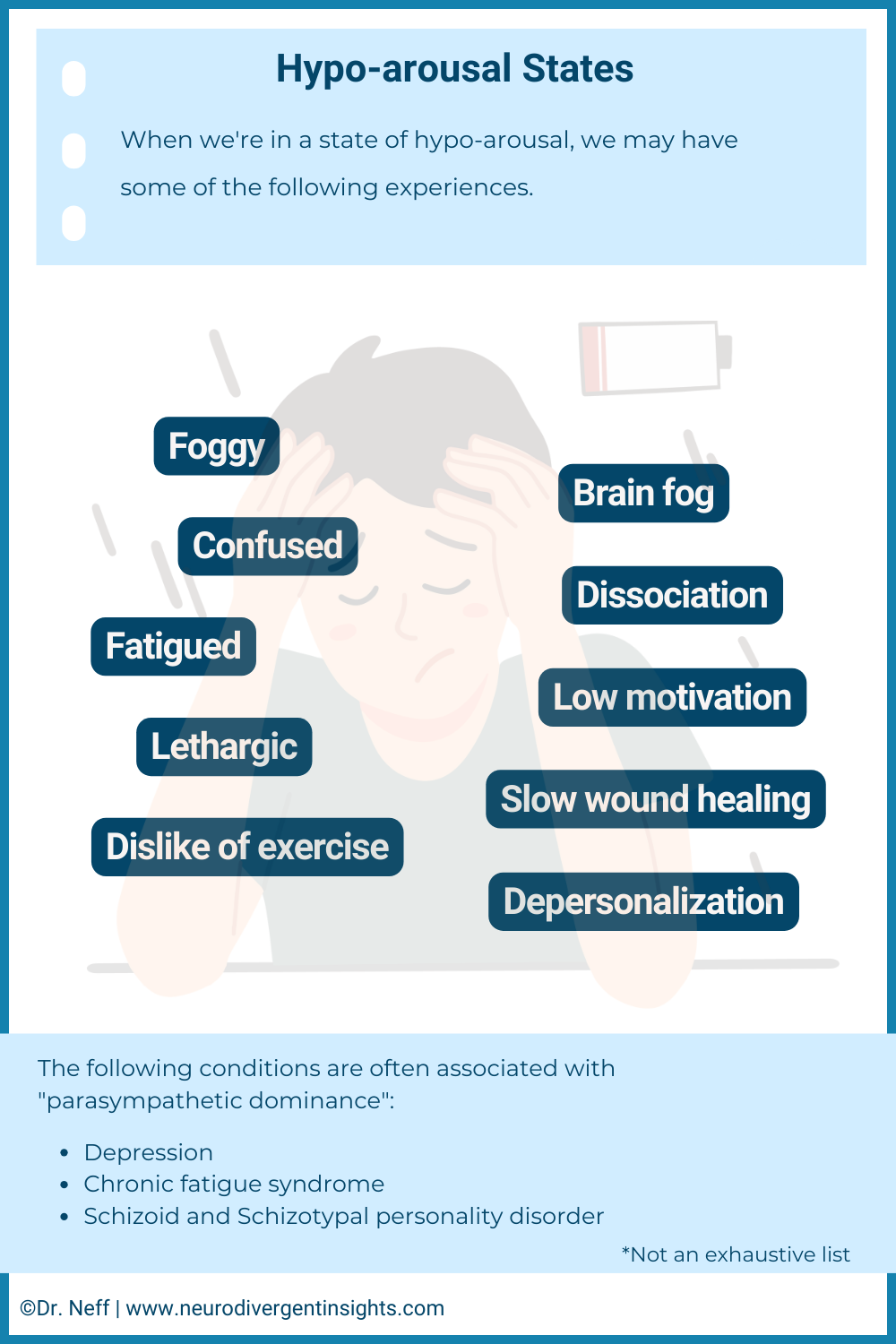
But what happens when we hit a stressful situation? It's like pressing the gas pedal too hard, revving the engine into overdrive (this is called hyperarousal), and we might start to feel anxious or panicky. On the other hand, sometimes our system does the opposite and goes into what's known as a dorsal shutdown mode. Think of it as the brakes being slammed! This is hypoarousal, where our overall alertness and energy drop.
This state of hypoarousal can manifest in numerous ways, such as feeling paralyzed or detached, experiencing a sense of numbness or a lack of emotion, and even physical collapse. Mental health conditions like depression, schizoid or schizotypal personality disorder, and dissociative disorders are often associated with a dominance of hypoarousal. In contrast, conditions such as anxiety and OCD tend to be more sympathetic-dominant, characterized by heightened arousal.
Understanding hypoarousal reveals how Dorsal Vagal Shutdown acts as a complex, protective strategy beyond typical stress responses.
Why a Dorsal Vagal Shutdown Happens
Dorsal Vagal Shutdown serves as the body’s emergency "freeze" response in the face of overwhelming stress or trauma, when the usual "fight or flight" reactions are not viable options. This protective measure conserves energy by minimizing metabolic activity and visibility to potential threats, a response managed by the dorsal vagal complex within the parasympathetic nervous system. It’s a primal survival strategy, putting the body into a temporary state of stasis to weather extreme stress or danger.
Now that we have a deeper understanding of the mechanisms involved in Dorsal Vagal Shutdown, it's important to understand the signs of Dorsal Vagal Shutdown. This way, we can better support ourselves and each other when facing this form of deep stress.
Symptoms of a Dorsal Vagal Shutdown
Dorsal Vagal Shutdown, a natural defense mechanism against overwhelming stress or trauma, can manifest through a variety of symptoms, signaling the body’s and mind's attempts to protect themselves. Understanding these symptoms can guide us in offering support and compassion to those experiencing them:
Fatigue: An overwhelming exhaustion not linked to physical exertion.
Dissociation: Feelings of detachment from reality, making it challenging to remain present.
Numbness and Emotional Flatness: A significant decrease in the ability to access or engage with emotions.
Cognitive Difficulties: Problems with focus, clarity of thought, and decision-making.
Physical Immobilization: A sensation of being “frozen” or unable to move.
Depression: Pervasive feelings of sadness, hopelessness, or despair.
Blackouts: Brief periods of unconsciousness or memory loss in severe cases.
Chronic Dorsal Vagal Shutdown
Beyond immediate support, it's crucial to address the enduring nature of Dorsal Vagal Shutdown for some individuals. Chronic Dorsal Vagal Shutdown can present a diffuse and persistent challenge, deeply affecting one's daily life and well-being. Understanding the differences between acute and prolonged responses highlights the importance of well-rounded treatment approaches. For Autistic people, experiencing Chronic Dorsal Vagal Shutdown can lead to significant challenges, including Autistic inertia and Autistic catatonia, affecting our ability to engage and respond.
Chronic Dorsal Vagal Shutdown is a prolonged state of hypoarousal or “freeze response” in response to stress or trauma, manifesting in symptoms like persistent fatigue, dissociation, emotional numbness, difficulty in thinking clearly, physical immobilization, depression, and, in some instances, blackouts. While these symptoms represent the body’s attempt to navigate extreme stress, they also significantly disrupt daily functioning.
Understanding that this condition signals deeper psychological issues, such as chronic stress or trauma, rather than being a disorder itself, is important. Treatment focuses on these underlying problems through therapy, medication, and lifestyle adjustments aimed at stress management and self-care.
It's equally important to rule out medical conditions that could mimic or exacerbate symptoms of Chronic Dorsal Vagal Shutdown. Conditions such as thyroid disorders, neurological issues, or vitamin deficiencies can present similar symptoms and should be considered in a comprehensive evaluation.
Seeking professional help is essential not only for therapeutic support but also for a thorough medical assessment to ensure a holistic approach to recovery. A mental health professional, in collaboration with medical practitioners, can help identify the root causes, whether they're psychological, physical, or a combination, and develop an effective treatment plan.
Difference Between Chronic and Acute Dorsal Vagal Shut Down
Dorsal Vagal Shutdown, known as the body's "freeze response" to overwhelming stress or trauma, is a natural and understandable reaction.This nervous system response can manifest in varying intensities and durations, leading to either acute or chronic states.
Acute Dorsal Vagal Shutdown is a temporary reaction to a specific stressor or traumatic event. This short-term response may last only a few hours or days, typically resolving as the individual processes the event and regains emotional and physiological balance. It's akin to the body hitting a "pause" button, allowing for a period of recovery before returning to normal functioning.
Chronic Dorsal Vagal Shutdown, in contrast, represents a prolonged state of hypoarousal that persists well beyond the immediate aftermath of a stressor or trauma. This extended shutdown can span weeks, months, or even longer, significantly affecting physical and mental health. It arises not as a standalone condition but as a symptom of ongoing issues, such as sustained stress, unresolved trauma, or other mental health challenges, indicating a deeper need for intervention.
The primary distinction between acute and chronic Dorsal Vagal Shutdown lies in their duration and the severity of their impact. While acute shutdown may serve as a temporary protective mechanism, chronic shutdown signals a profound disruption in how the body and mind manage and recover from stress.
How to Sooth a Dorsal Vagal Shutdown
Creating a safe, nurturing environment is crucial for anyone experiencing a Dorsal Vagal Shutdown. This involves not only physical safety but emotional safety, helping the person find a sense of stability and presence. If a person is in a deep state of shutdown you want them to slowly and gently come back into the body. Below are strategies to aid in upregulating the nervous system.
Engage in Grounding Techniques: Grounding techniques that focus on reconnecting with the present moment could involve tactile activities like holding a cold ice pack, touching various textures, or engaging in light, mindful exercises that gently activate the body without overwhelming it.
Create a Comforting Space: A quiet, comfortable environment can still be beneficial, allowing the individual to step back from overstimulation. However, this space should encourage gentle sensory engagement rather than complete isolation or sensory deprivation which might deepen the sense of dissociation.
Upregulate with Sensory Input: Leverage sensory inputs to delicately stimulate and awaken the senses, guiding the body back to a state of gentle alertness. This can include the use of soft, rhythmic music, visually calming elements like gentle videos or soft lamps, and the subtle invigoration from lightly scented oils. Additionally, consider the comforting grounding effect of a weighted blanket or the familiar scent of essential oils. Together, these sensory tools not only encourage reconnection with the environment but also assist in transitioning the nervous system towards a more relaxed and aware state, so also helps to restore a sense of agency and physical control.
Engage in Gentle Movement: Sometimes, gentle, mindful movement like walking, swaying or stretching, or yoga can help reconnect with one’s body and alleviate feelings of immobilization associated with the shutdown. This also helps to restore a sense of agency and physical control.
Therapeutic Touch: For some, therapeutic touch or self-massage with warm oils can be incredibly grounding. This tactile engagement can help reaffirm the body’s presence and capacity for sensation, aiding in the gradual reconnection process. For those with low tolerance for touch, weighted items can serve a similar function.
Seek Professional Support: In cases where the shutdown is intense or persistent, consulting a mental health professional is advisable. They can offer tailored strategies for coping and addressing underlying triggers, facilitating a deeper healing process.
It’s essential to approach recovery from a Dorsal Vagal Shutdown with patience and compassion to self and others. The journey back from such a profound state of disconnection is delicate and may require time and gentle exploration of what strategies feel most supportive.
Sensory Shutdowns and Dorsal Vagal Shutdown
Sensory overload can often lead to sensory shutdown, a condition where the nervous system reduces sensory processing in response to overwhelming input. This can precede or trigger a Dorsal Vagal Shutdown, marking a deeper state of conservation to manage stress. When sensory overload is too intense, the nervous system may opt for a Dorsal Vagal Shutdown to protect the individual, reducing both sensory perception and overall bodily function. Recognizing impending sensory overload and employing strategies like using sensory supports or setting boundaries around sensory input can help mitigate the transition into a more extensive shutdown state. You can read more about sensory regulation over here.
Resources
Vagal Nerve Stimulators: Using a vagal nerve stimulator helps to strengthen your vagal tone which improves the flexibility of your nervous system! My personal favorite is the sensate. Use code NeuroInsights to get 10% off.
Biofeedback: 59 Breaths is a biofeedback program designed to improve heart rate variability and nervous system flexibility. (Note only works with Apple Watch). Use this link to get $20 off the annual subscription.
Workbook: For more of a deep dive on the nervous system you can check out the Neurodivergent Nervous System digital workbook here.
Free Blog Posts: I have several free blog posts up on nervous system regulation practices and strategies.
Polyvagal Theory: Much of the information we have on dorsal vagal shutdown comes from polyvagal theory. The Polyvagal Flip Chart is a visually accessible and helpful way to understand the basics.
Summary: Dorsal Vagal Shutdown
Dorsal Vagal Shutdown, also known as Hypoarousal, is a type of "freeze response" that occurs in the face of overwhelming stress or trauma. It's a natural and normal response that allows our bodies to conserve energy and protect ourselves when we are unable to fight or flee. Symptoms of Dorsal Vagal Shutdown can include fatigue, dissociation, numbness, foggy mind, immobilization, depression, dissociation, and even blackouts. It's important to create a safe and supportive environment for someone experiencing Dorsal Vagal Shutdown, and to encourage them to seek professional help if necessary. By providing understanding and support, we can help each other navigate through these difficult times and come out stronger on the other side.
References
Gourine, A. V., & Ackland, G. L. (2019). Cardiac vagus and exercise. Physiology, 34(1), 71-80.
Porges, S. W. (2001). The polyvagal theory: phylogenetic substrates of a social nervous system. International journal of psychophysiology, 42(2), 123-146.
Spratt, E. G., Nicholas, J. S., Brady, K. T., Carpenter, L. A., Hatcher, C. R., Meekins, K. A., ... & Charles, J. M. (2012). Enhanced cortisol response to stress in children in autism. Journal of autism and developmental disorders, 42, 75-81.