What is the Connection Between ADHD and OCD?
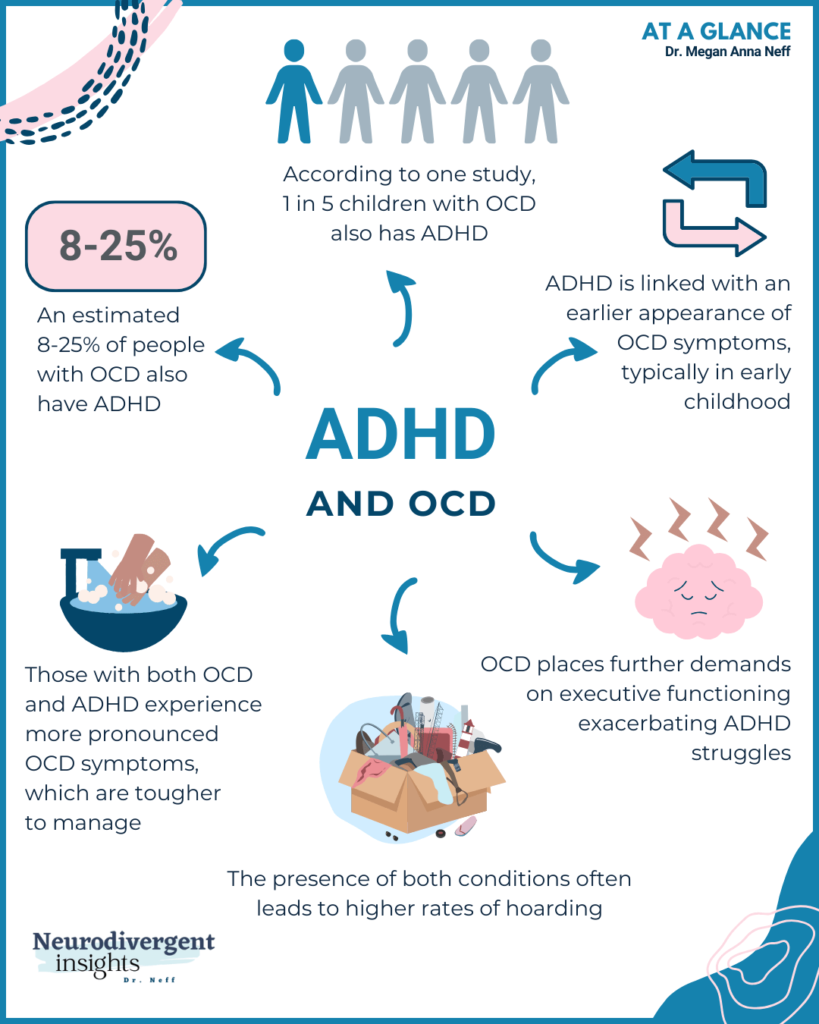
Have you ever wondered about the connection between Attention Deficit Hyperactivity Disorder (ADHD) and Obsessive Compulsive Disorder (OCD)? As an ADHDer who struggled with OCD in childhood, I understand firsthand how these two conditions can intersect. And as a psychologist who has worked with numerous individuals with ADHD and OCD, I have seen the impact that their co-occurrence can have on a person’s daily life. With that in mind, the intention of creating this infographic was to provide accessible information about the potential overlap between ADHD and OCD.
With that in mind, this blog post will review some of the research findings regarding the co-occurrence of OCD and ADHD, the implications of co-occurrence, and treatment considerations. Additionally, you can read more about symptom overlap and potential misdiagnosis, see my Misdiagnosis Monday post here.
The Overlap Between ADHD and OCD: Understanding the Prevalence Rates
The co-occurrence of Obsessive Compulsive Disorder (OCD) and Attention Deficit Hyperactivity Disorder (ADHD) is not uncommon, with several studies highlighting the overlap between these two conditions. Here are some of the key findings:
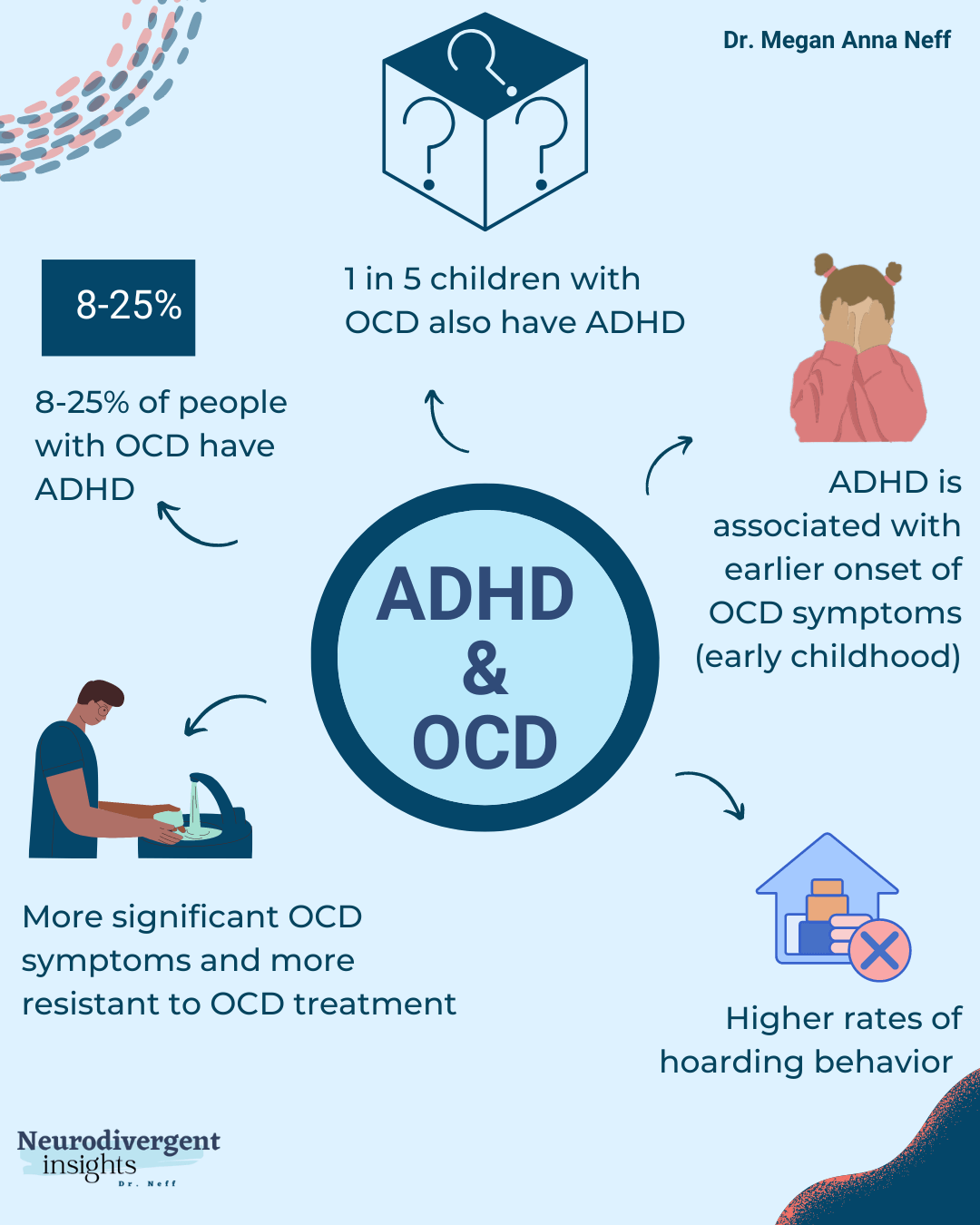
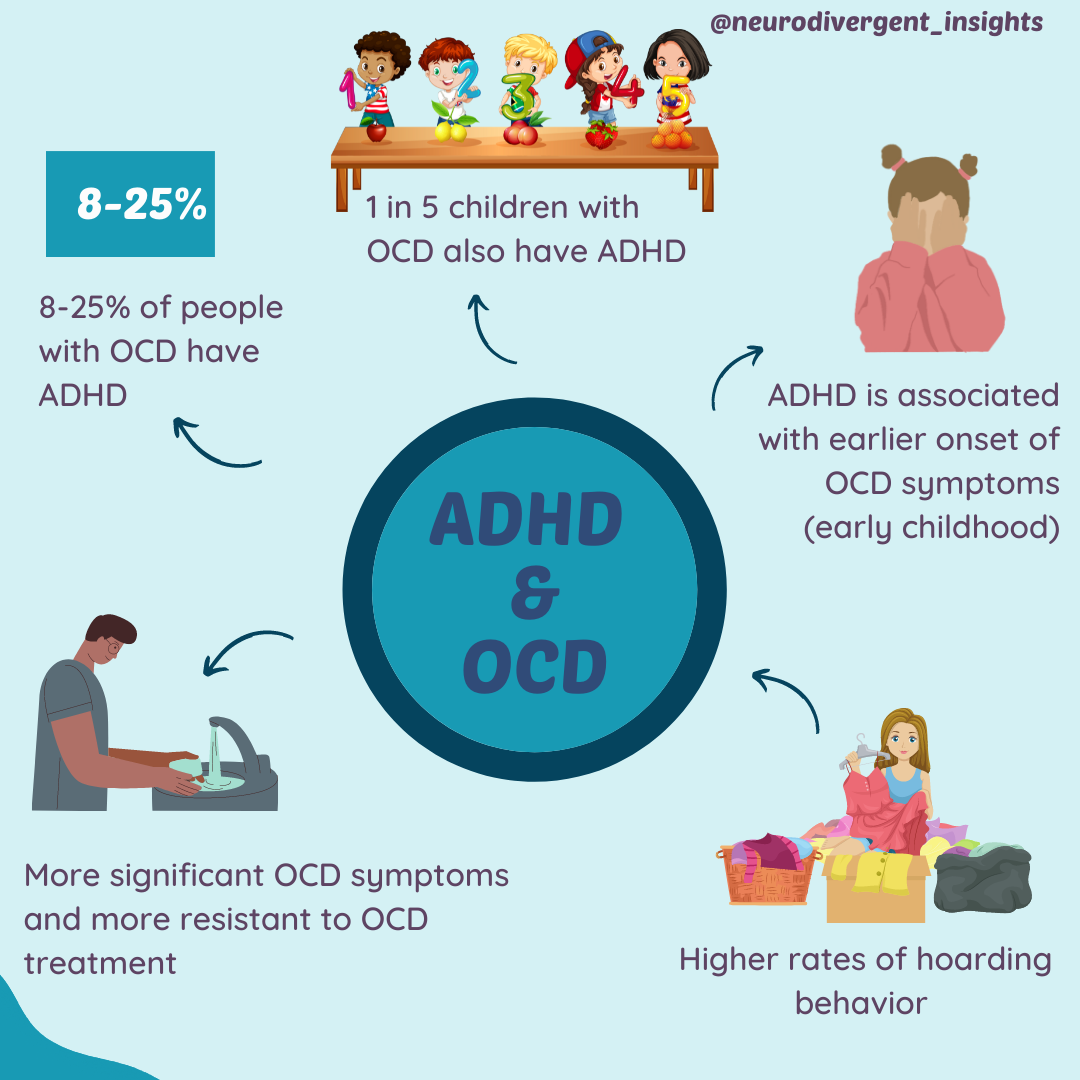
1 in 5 children with OCD had co-occurring ADHD (Abramovitch and Mittelman; 2013).
1 in 12 adults with OCD has co-occurring ADHD (although it is speculated that ADHD is underdiagnosed among OCD adults, particularly those with ADHD-inattentive type) (Olivardia, 2021).
8-25% of people with OCD also have ADHD (Brem et al., 2014).
ADHD has been shown to be the most common co-occurring condition among early-onset OCD (Brem et al., 2014).
A study involving 94 children and adolescents with OCD found that 25.5% had co-occurring ADHD, and a second study in 2010 found that 17.1% had co-occurring OCD-ADHD (Masi, 2006; Masi, 2010).
In a study involving 155 OCD-affected individuals (aged 4-82), 11.8% met definite criteria for ADHD, and an additional 8.6% had probable ADHD (a total of 20.4%) (Geller et al., 2007).
ADHD and OCD: Understanding the Implications of Co-Occurrence
The co-occurrence of ADHD and OCD can have significant implications for diagnosis and treatment. Here are some of the key findings:
People with ADHD and OCD typically have an earlier onset of OCD symptoms, often in early childhood (Walitza et al. 2008).
Co-occurring ADHD is associated with more severe OCD symptoms, and people with both conditions demonstrate more “treatment resistance” for OCD (Masi, 2010; Walitza et al. 2008).
Co-occurrence is also correlated with more hoarding behavior (41.9% compared to 29.2% of non-ADHD people with OCD) (Sheppard et al., 2010).
These findings suggest that people with both conditions may experience more severe symptoms and resistance to treatment, highlighting the importance of tailored interventions that take into account the specific needs of individuals with ADHD and OCD. There is a need for further research to better understand the relationship between ADHD and OCD, and to develop more effective treatments for those affected by both conditions.
Treating Co-Occurring ADHD and OCD: Unique Considerations
When treating co-occurring ADHD and OCD, it’s important to consider the unique challenges that arise from the interaction between the two conditions. As mentioned earlier, ADHD is associated with dopamine disruption, and OCD with serotonin disruption. This means that different pharmaceutical interventions are often required for each condition. The most common medical intervention for OCD is an antidepressant (SSRI), which helps boost serotonin in the brain. Stimulant medication, often used for ADHD treatment, may also help reduce ADHD symptoms, but can sometimes increase OCD symptoms.
In addition to medication, psychological treatments such as Cognitive Behavioral Therapy (CBT) and Exposure and Response Prevention (ERP) are commonly used to treat OCD. However, ADHDers may struggle more with exposure therapies, which involve facing anxiety-inducing situations or stimuli to help overcome OCD symptoms. This is because exposure therapy often requires sustained attention and inhibitory control, which are common areas of difficulty for people with ADHD.
It’s important to consider sensory needs when developing a treatment plan for ADHD and OCD. Some ADHDers are particularly sensitive to sensory input, which can exacerbate anxiety and OCD symptoms. Incorporating sensory breaks, such as time away from overwhelming stimuli or the use of fidget toys, can be helpful in managing symptoms. Additionally, visual aids and education can be beneficial for the high-visual ADHD brain.
Overall, the treatment of co-occurring ADHD and OCD can be complex and requires a thorough assessment of each person’s unique needs. Treatment plans should be tailored to the individual and may require ongoing monitoring and adjustments to achieve the best outcomes.
Key Takeaways: Understanding and Treating ADHD-OCD Co-Occurrence
Co-occurring ADHD and OCD is a complex and challenging combination, with high prevalence rates and unique implications for diagnosis and treatment. Despite the symptom overlap between the two conditions, research suggests that they are distinct disorders with different underlying brain mechanisms. However, the presence of both conditions can exacerbate symptoms, leading to more severe impairments and greater treatment resistance.
When assessing and treating ADHD-OCD co-occurrence, it’s important to consider the unique challenges that arise from the interaction between the two conditions. This includes taking into account the prevalence rates of co-occurrence, the implications for diagnosis and treatment, and the importance of addressing the sensory needs and high-visual learning style of the ADHD brain. Effective treatment strategies may include a combination of medication, therapy, and lifestyle modifications tailored to the individual’s needs.