How Do ADHD and PTSD Overlap?
Have you ever wondered how ADHD and PTSD overlap? It turns out that they co-occur at really high rates, but there’s still a lot we don’t understand about this connection. What we do know is that having ADHD can make someone more vulnerable to developing PTSD, and when they occur together, it’s known as “complex ADHD.” And let me tell you, that can make things even more complicated for the person dealing with it.
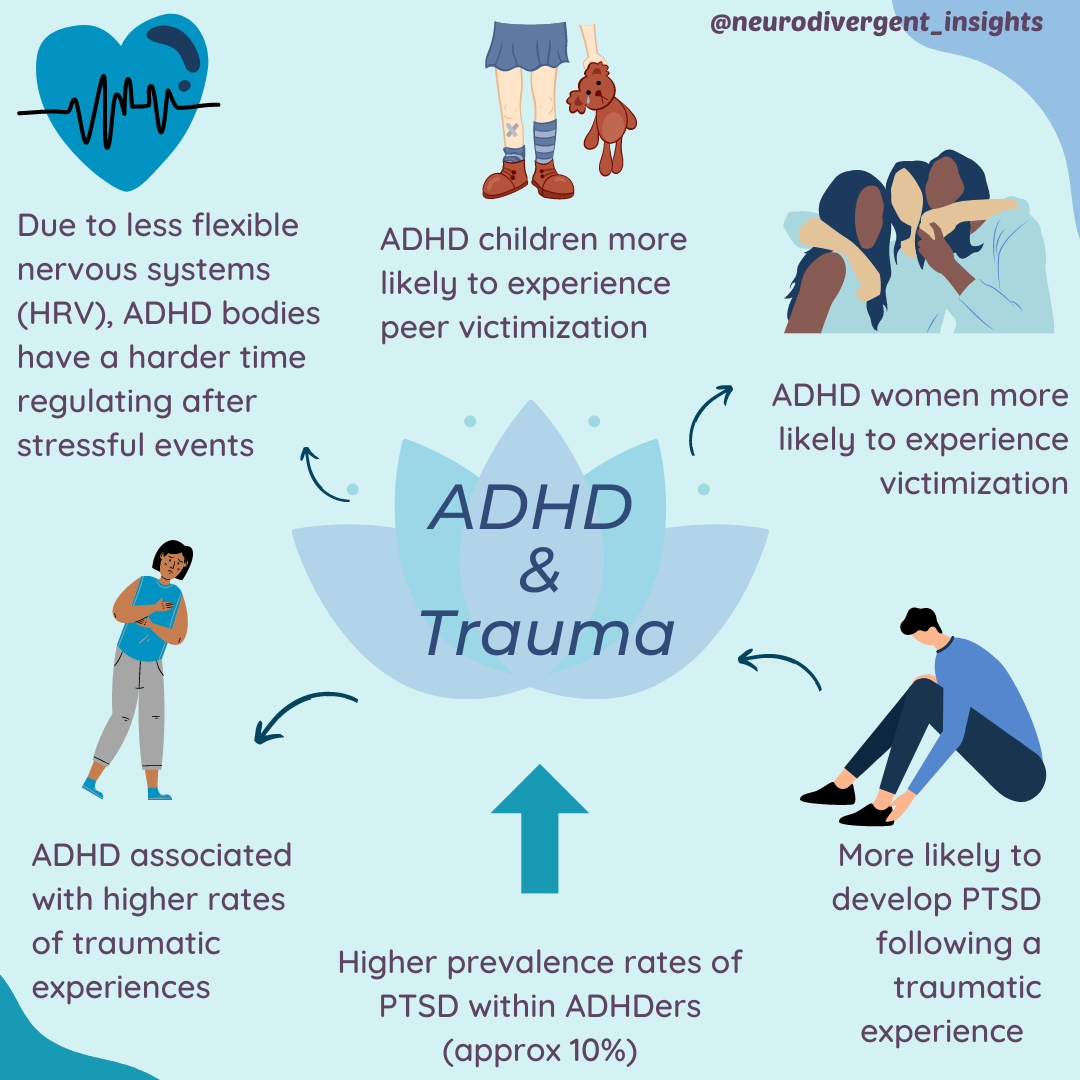
You may be wondering how frequently PTSD and ADHD co-occur. Unfortunately, true estimates are difficult to discern due to factors such as misdiagnosis and undiagnosed cases. The prevalence rates also vary greatly among different populations. For instance, one study (El Ayoubi et al., 2020) found that 84% of ADHDers receiving inpatient substance abuse treatment had co-occurring PTSD, while Antshel et al. (2013) found that 10% of people with ADHD had PTSD (compared to 1.6% of the general population).
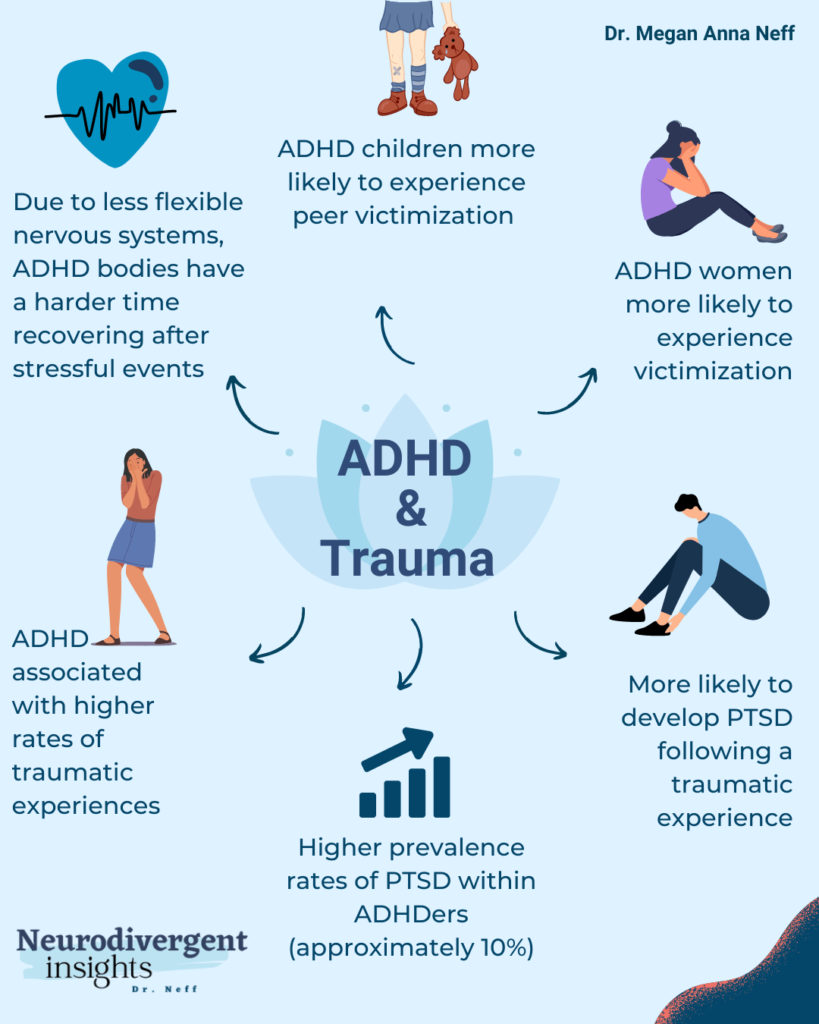
So why do ADHD and PTSD co-occur so frequently? Well, according to studies by Adler et al., (2004) and Kessler et al. (2006), ADHD is actually a risk factor for developing PTSD. But there are a few other factors that contribute to this overlap too. For one, people with ADHD are at a higher risk for experiencing traumatic events in the first place ((Ford et al., 2009). Plus, our nervous systems are more sensitive, which means that traumatic events can hit us even harder and make us more likely to develop PTSD (Biederman et al., 2012), And finally, according to Crenshaw and Mayfield, (2021), early life trauma can act as a trigger for those who are genetically predisposed to ADHD.
All in all, there’s a lot to unpack when it comes to the overlap between ADHD and PTSD. But by understanding these factors, we can work towards better support and treatment for those dealing with this “complex ADHD” combo.
ADHD Risk Factors for Trauma & PTSD
People with ADHD are known to have an elevated risk for exposure to traumatic experiences, which may make them more susceptible to developing post-traumatic stress disorder (PTSD). This section explores some of the factors that contribute to this increased risk, including the prevalence of victimization among ADHDers, the complex relationship between ADHD and intimate partner violence (IPV), and the emerging research on the nervous system of people with ADHD.
ADHDers Have a Higher Likelihood of Experiencing Trauma
ADHDers have an elevated risk of exposure to traumatic experiences, which can increase their likelihood of developing PTSD (Ford et al., 2009). In fact, ADHD women have an even higher risk of victimization than their non-ADHD counterparts. For instance, studies by Synder (2015) found that college women with ADHD experience victimization at significantly higher rates than non-ADHD women. Similarly, ADHD children are more likely to be victims of peer victimization than non-ADHD children, as shown in studies by Elfron et al. (2021) and Fogleman et al., (2018).
ADHDers and Intimate Partner Violence
When it comes to intimate partner violence (IPV), the research is more complex, with studies showing both elevated rates of perpetration of IPV and of victimization of IPV among ADHDers (Wymbs et al., 2017).
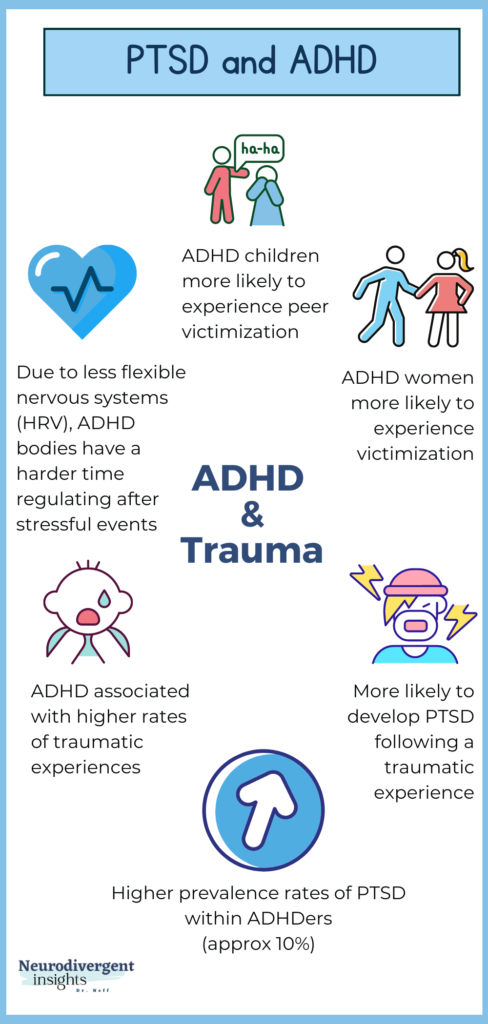
The ADHD Nervous Systems
Emerging research is also examining the nervous system of ADHDers. Studies by Raghurama Rukmani et al. 2016 found that ADHD children had low HRV variability and a tendency towards sympathetic dominance (fight-or-flight response) in their nervous systems, which can make it harder to regulate after stressful events. This can increase vulnerability to heightened stress responses, leading to emotional and physiological difficulties. This may also be one of the underlying mechanisms for why a person with ADHD is more likely to experience a stressful event as traumatic compared to non-ADHDers.
Implications for Co-Occurring PTSD and ADHD
When ADHD and PTSD co-occur, both conditions tend to exacerbate the symptoms of the other. This can lead to a significant amount of overlap and make it difficult to identify when both conditions are present, resulting in one diagnosis being missed. It is important to treat both conditions simultaneously to improve the person’s symptoms.
One of the most effective strategies for managing both ADHD and PTSD is a combination of medication and therapy. Here are some recommendations to consider:
Medication: Stimulant and behavioral strategies work well for ADHD and trauma-focused psychotherapy has been shown to be effective for PTSD.
Information is mixed when it comes to stimulant use. For some stimulant use may exacerbate anxiety symptoms associated with PTSD. However, in some cases, stimulants can be useful in the context of PTSD. One pilot study found positive results of stimulant use in the context of PTSD (McAllister et al., 2015). And stimulant use may help with focus and attention issues which will help a person more fully work through their trauma.
On the other hand, stimulants may not be appropriate for everyone with PTSD, as they can activate the nervous system and intensify hypervigilance and anxiety. When stimulants are not indicated other medications may be considered such as SNRIs which have also shown promise to help reduce symptoms of ADHD/PTSD (Lowry, 2021). Given the complexity and attention to nervous system activation, it is recommended to work closely with a prescriber and therapist when establishing the ideal pharmaceutical support.
Other medications, such as SNRIs, have shown promise for reducing symptoms of both ADHD and PTSD.
Because of the complexity of the nervous system and how these medications work, it’s important to work closely with a prescriber to determine the best medication regimen.
Therapy: Evidence-based therapies for PTSD, such as cognitive-behavioral therapy and eye movement desensitization and reprocessing, can also be helpful for individuals with co-occurring ADHD.
Lifestyle modifications, such as exercise and mindfulness practices, can also be beneficial in managing symptoms of both conditions.
It’s important for individuals with co-occurring ADHD and PTSD to work closely with their medical team to ensure the best treatment plan is being used for both conditions.
Having a thorough understanding of the co-occurrence of ADHD and PTSD can help healthcare providers and patients work together to develop effective treatment strategies that address both conditions.
Further Resources
Trauma Resources for Clinicians
CE Webinars and Certificate Courses
Featuring Stephen Porges, Peter Levine, Linda Curran, Richard Schwartz, Janina Fisher, and more!
Certificate: Certified Clinical Trauma Professional Level 1
Good for clinicians wanting comprehensive training in trauma
Great for clinicians working with teenagers or others wanting to integrate special interests, passions, superheros or pop culture into their work with teens and young adults.
Trauma Resources for Individuals
Self-Care Tips and Trauma: This website provides several helpful strategies for coping with PTSD.
Psychological First Aid: The VA provides several manuals and handouts with lots of great resources and interventions for treating people in the aftermath of trauma.
Grounding: Utilizing grounding techniques is foundational in trauma work. Check out my free PDF with grounding exercises and info.
Sensory Soothers: Consider having extra sensory soothers and fidgets around the house to access energy. Fidgets can also function to help with tactile grounding.
ADHD workbooks or check out my collection of ADHD favorite books
Or check out some of my favorite executive function helpers or sleep supports
References
Adler, L. A., Kunz, M., Chua, H. C., Rotrosen, J., & Resnick, S. G. (2004). Attention-Deficit/Hyperactivity Disorder in adult patients with Posttraumatic stress disorder (PTSD): Is ADHD a vulnerability factor? Journal of Attention Disorders, 8(1), 11–16. https://doi.org/10.1177/108705470400800102
Biederman, J., Petty, C. R., Spencer, T. J., Woodworth, K. Y., Bhide, P., Zhu, J., & Faraone, S. V. (2013). Examining the nature of the comorbidity between pediatric attention deficit/hyperactivity disorder and post-traumatic stress disorder. Acta Psychiatrica Scandinavica, 128(1), 78–87. https://doi.org/10.1111/acps.12011
Efron, D., Wijaya, M., Hazell, P., & Sciberras, E. (2021). Peer Victimization in Children With ADHD: A Community-Based Longitudinal Study. Journal of attention disorders, 25(3), 291–299. https://doi.org/10.1177/1087054718796287
El Ayoubi, H., Brunault, P., Barrault, S., Maugé, D., Baudin, G., Ballon, N., & El-Hage, W. (2020). Posttraumatic Stress Disorder Is Highly Comorbid With Adult ADHD in Alcohol Use Disorder Inpatients. Journal of attention disorders, 1087054720903363.
Fogleman, N.D., Slaughter, K.E., Rosen, P.J. et al. Emotion regulation accounts for the relation between ADHD and peer victimization. J Child Fam Stud 28, 2429–2442 (2019). https://doi.org/10.1007/s10826-018-1297-8
Ford, J.D., Connor, D.F. (2009). ADHD and posttraumatic stress disorder. Curr Atten Disord Rep 1, 60–66. https://doi.org/10.1007/s12618-009-0009-0
McAllister, T. W., Zafonte, R., Jain, S., Flashman, L. A., George, M. S., Grant, G. A., He, F., Lohr, J. B., Andaluz, N., Summerall, L., Paulus, M. P., Raman, R., & Stein, M. B. (2016). Randomized Placebo-Controlled Trial of Methylphenidate or Galantamine for Persistent Emotional and Cognitive Symptoms Associated with PTSD and/or Traumatic Brain Injury. Neuropsychopharmacology : official publication of the American College of Neuropsychopharmacology, 41(5), 1191–1198. https://doi.org/10.1038/npp.2015.282
Rukmani, M. R., Seshadri, S. P., Thennarasu, K., Raju, T. R., & Sathyaprabha, T. N. (2016). Heart Rate Variability in Children with Attention-Deficit/Hyperactivity Disorder: A Pilot Study. Annals of neurosciences, 23(2), 81–88. https://doi.org/10.1159/000443574
Snyder J. A. (2015). The Link Between ADHD and the Risk of Sexual Victimization Among College Women: Expanding the Lifestyles/Routine Activities Framework. Violence against women, 21(11), 1364–1384. https://doi.org/10.1177/1077801215593647
Wymbs, B. T., Dawson, A. E., Suhr, J. A., Bunford, N., & Gidycz, C. A. (2017). ADHD Symptoms as Risk Factors for Intimate Partner Violence Perpetration and Victimization. Journal of interpersonal violence, 32(5), 659–681. https://doi.org/10.1177/0886260515586371