DSM-5 Criteria for ADHD Explained (In Picture Form)
DSM-5 In Picture Form: ADHD
I am back with week 3 of my DSM-5 in pictures series (if you missed it you can check out last week’s post on autism here).
Disclaimers, FAQs, and Basic Information on the DSM-5
Why am I creating this series: I am creating this series to increase the accessibility and transparency of the DSM-5 and the clinical tools people like me use when we are giving you (or anyone) a diagnosis. I find the mental health world can be overly mysterious, increasing anxiety and stress for many. I believe this process should be as understandable and transparent as possible. I am using visuals to break down the DSM-5 because, like many neurodivergent people, unless a thing is visual, I have a hard time understanding it!
Disclaimers: This is for educational purposes only and isn’t intended as a substitute for medical advice or to be used as a primary diagnostic tool.
A word on language: I use direct language from the DSM. This is for educational purposes. Much of the language used is deficit-based and pathological in nature. It doesn't mean I agree with all the wording (in fact, I do not!). I have made this choice to increase the transparency of what is actually in the DSM.
What do A, B, and C mean? The DSM is broken into different criteria buckets. While a person doesn't need to have all symptoms of each criterion, they typically need to have all criteria met (A, B, C, etc..) to be diagnosed.
What about international people? The DSM-5 is based in the United States (the Psychological Association of America puts it out). However, the criteria are very similar to the ICD, which is used globally and broadly in medical settings.
Okay, now that we’ve gone over the purpose, intent, and limits of this post. Let’s dive in!
The DSM-5 Criteria for ADHD
To meet the criteria for ADHD, five buckets of diagnostic criteria must be met (A-E). The ones that we spend the most time with are criteria A. Criteria A is split into two subcategories (inattention and hyperactivity). Within each subcategory are nine symptoms. For a diagnosis of ADHD, a person must experience 6 of the nine symptoms. The other criteria are largely used to help differentiate ADHD from other conditions and/or diagnoses.
ADHD Criteria A
ADHD Criteria Subcategory A-Inattentive Type
Criteria A subcategory 1 includes inattentive traits. According to the DSM, inattention criteria are met if: "Six (or more) of the following symptoms have persisted for at least 6 months to a degree that is inconsistent with developmental level and that negatively impacts directly on social and academic/occupational activities." [Note for people 17 and older only five traits have to be present to meet the criteria]
One of the critical components of the above sentence is that the inattentiveness must either 1) be inconsistent with developmental level (meaning significantly different than peers or 2) must impact the person negatively (in work, school, etc.). This is an essential aspect of what distinguishes ADHD from everyday inattentiveness.
Everyone has moments of inattention, distractibility, and difficulty with focus. What distinguishes ADHD from situational struggles is that it is a part of a person's baseline experience and is not situation-dependent (it is present across multiple contexts). If a person only struggles with attention and focus when in a chaotic or distracting environment, that isn't ADHD; that is situational inattention.
Throughout the COVID pandemic, there has been a lot of confusion regarding ADHD. Attention became much more difficult for many people when we lost our framework for work, and our home/work boundaries collapsed. We lost the structures that primed our brains for focus and attention. Attention and focus got a lot harder!
Many people began experiencing struggles with inattention; however, if it wasn't present until the pandemic, it was situational inattention. The anxiety that came with a global pandemic also negatively impacted focus for many people. These are examples of situational inattention rather than ADHD. So, on the one hand, many people may have falsely concluded they were ADHDers. However, at the same time, the pandemic also enabled many undiagnosed ADHDers to discover their ADHD for the first time.
Many ADHDers who mask their ADHD who could scrape by with the structures and compensatory strategies they had in place all of a sudden burned out and collapsed with the added pressures of the pandemic. [Sidenote, it is not uncommon for ADHD to go undiagnosed until the stressors overpower the coping strategies, for example, after the birth of a child or going to graduate school are common times for a high-achieving ADHDer to first get diagnosed because their stressors have exceeded their ability to cope]. So to summarize, during the pandemic, more people are struggling with inattention and may falsely believe they are ADHDers. Also, more people accurately understand their ADHD for the very first time in their life! And simultaneously, we have seen a wave of ADHD awareness across social media platforms. As I said, it's led to a lot of ADHD confusion!
The conflation of these factors has led to a lot of skepticism and confusion. I regularly hear cynical professionals say, "everyone thinks they're ADHD now." While people struggling with situational inattention due to the pandemic is certainly a portion of people coming in for ADHD evaluations. I also believe a significant portion is, in fact, ADHDers whose coping strategies were simply exhausted once boundaries and structure collapsed and who have been empowered through ADHD advocacy and education.
The last paragraph was a bit of a divergent rabbit trail. Divergent thinking and thought processes that interweave ideas are also a core feature of ADHD; it's just not on the DSM list. Some clinicians may look at non-linear thought processes as "tangential," (tangential thought processes are often associated with ADHD). However, if you take a closer look, we often connect and interweave our ideas. It's not linear, but it is often purposeful. Our tendencies to interweave ideas also contributes to inattention. Internally we may go on a rabbit trail in our mind when we hear someone telling a story. This may cause us to lose focus on the conversation because our divergent mind has taken us elsewhere. On the outside, this looks like inattention. However, I prefer to think about this as difficulty regulating our attention. Our curiosity has simply taken us elsewhere, and our attention has gone along with it.
Back to the DSM. To meet the criteria for ADHD-inattentive type, a person must have six of the following nine attentive traits (the following is direct text and language of the DSM-5).
Often fails to give close attention to details or makes careless mistakes in schoolwork, at work, or during other activities (e.g., overlooks or misses details, work is inaccurate).
Often has difficulty sustaining attention in tasks or play activities (e.g., has difficulty remaining focused during lectures, conversations, or lengthy reading).
Often does not seem to listen when spoken to directly (e.g., mind seems else where, even in the absence of any obvious distraction).
Often does not follow through on instructions and fails to finish schoolwork, chores, or duties in the workplace (e.g., starts tasks but quickly loses focus and is easily sidetracked).
Often has difficulty organizing tasks and activities (e.g., difficulty managing sequential tasks; difficulty keeping materials and belongings in order; messy, disorganized work; has poor time management; fails to meet deadlines).
Often avoids, dislikes, or is reluctant to engage in tasks that require sustained mental effort (e.g., schoolwork or homework; for older adolescents and adults, preparing reports, completing forms, reviewing lengthy papers).
Often loses things necessary for tasks or activities (e.g., school materials, pencils, books, tools, wallets, keys, paperwork, eyeglasses, mobile telephones).
Is often easily distracted by extraneous stimuli (for older adolescents and adults, may include unrelated thoughts).
Is often forgetful in daily activities (e.g., doing chores, running errands; for older adolescents and adults, returning calls, paying bills, and keeping appointments).
When looking through the list of inattention, it’s important to remember that the DSM is written from the outside. The DSM captures external observations and behaviors and rarely captures internal experiences. The “symptoms” listed under ADHD are observed from the external observer and don’t necessarily align with the internal experience.
For example, the first criterion for ADHD inattentiveness includes “making careless mistakes.” To the outside observer, these mistakes may look careless; however, rarely are these experienced as careless for the ADHDer. I recently talked about this over on Instagram, and there are lots of great comments from ADHDers who share similar feelings about the use of the word “careless” here.
Before leaving the topic of inattention, it’s important to note the interest-based nervous system. Many of these struggles are not present when we engage in high-interest activities. When we are interested in a topic (or it’s challenging, novel, or urgent), this increases our dopamine, impacting our ability to focus (dopamine helps our neurons talk to each other more efficiently, which is why it helps with attention and focus). For this reason, I believe it is more accurate to describe ADHD as “difficulty regulating attention” vs. “attention-deficit disorder.”
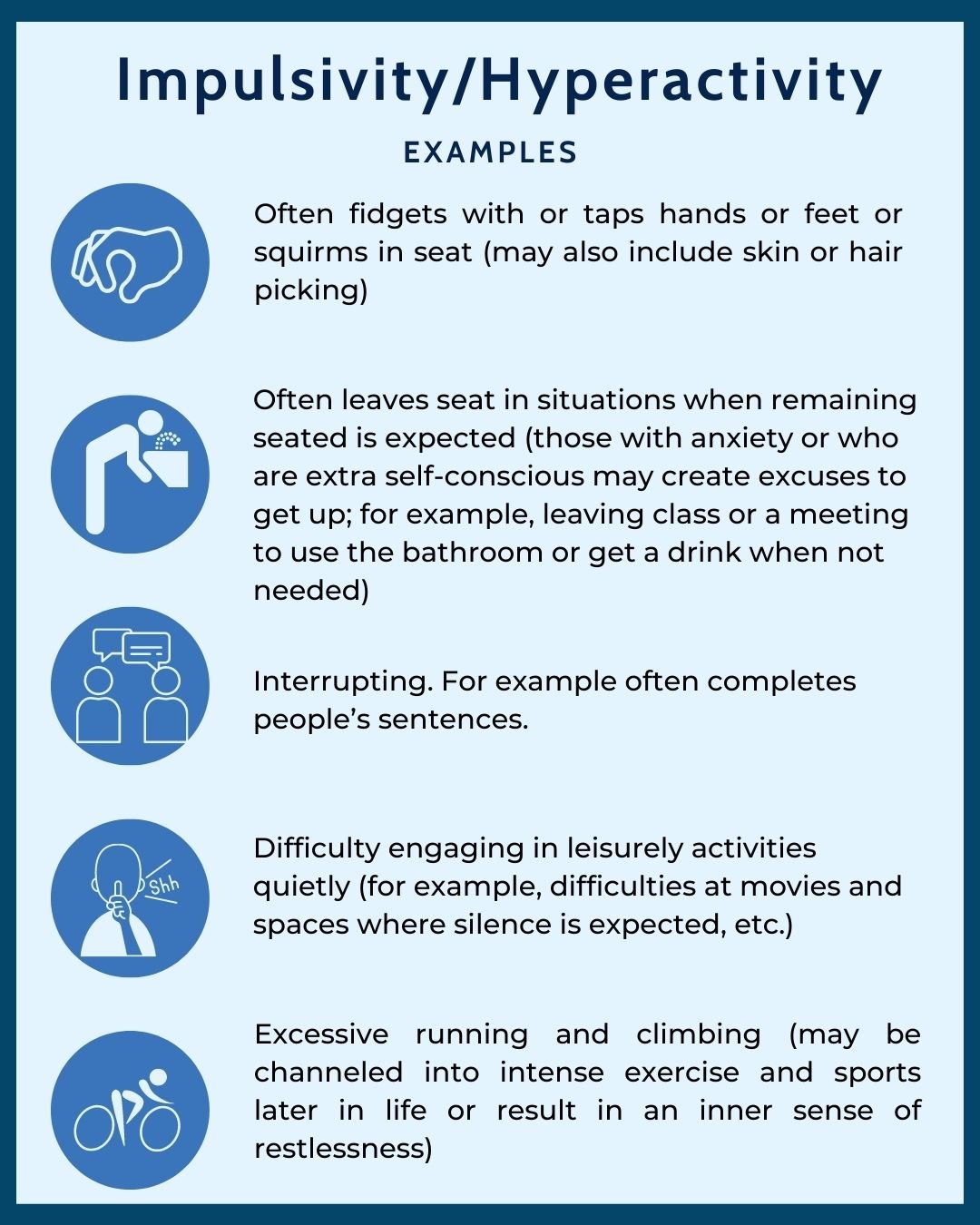
ADHD Criteria Subcategory B-Hyperactivity and Impulsivity
The second subcategory of criteria A refers to hyperactivity and impulsivity. There are nine symptoms outlined in the DSM. Six symptoms need to be present (for six months) and cause difficulties at work, school, or in relationships (for people 17 and older only five symptoms need to be present).
The following is direct text and language of the DSM-5).
Often fidgets with or taps hands or feet or squirms in seat.
Often leaves seat in situations when remaining seated is expected (e.g., leaves their place in the classroom, in the office or other workplace, or in other situations that require remaining in place).
Often runs about or climbs in situations where it is inappropriate. (Note: In adolescents or adults, may be limited to feeling restless.)
Often unable to play or engage in leisure activities quietly.
Is often “on the go,” acting as if “driven by a motor” (e.g., is unable to be or uncomfortable being still for extended time, as in restaurants, meetings; may be experienced by others as being restless or difficult to keep up with).
Often talks excessively.
Often blurts out an answer before a question has been completed (e.g., completes people’s sentences; cannot wait for a turn in conversation).
Often has difficulty waiting their turn (e.g., while waiting in line).
Often interrupts or intrudes on others (e.g., butts into conversations, games, or activities; may start using other people’s things without asking or receiving permission; for adolescents and adults, may intrude into or take over what others are doing).
One critique of the DSM criteria for hyperactivity is that it overly focuses on external behavior and doesn’t consider hyperactivity turned inward.
Hyperactivity can also be turned inward and internalized. This is more difficult to assess and capture. Particularly given the DSM criteria for ADHD is behavior-based, it can be more challenging to detect hyperactivity that has been turned inward (to assess for this, you have to get at the subjective experience of the person). Inward-facing hyperactivity often results in anxiety, intense rumination, and a sense of internal agitation/restlessness.
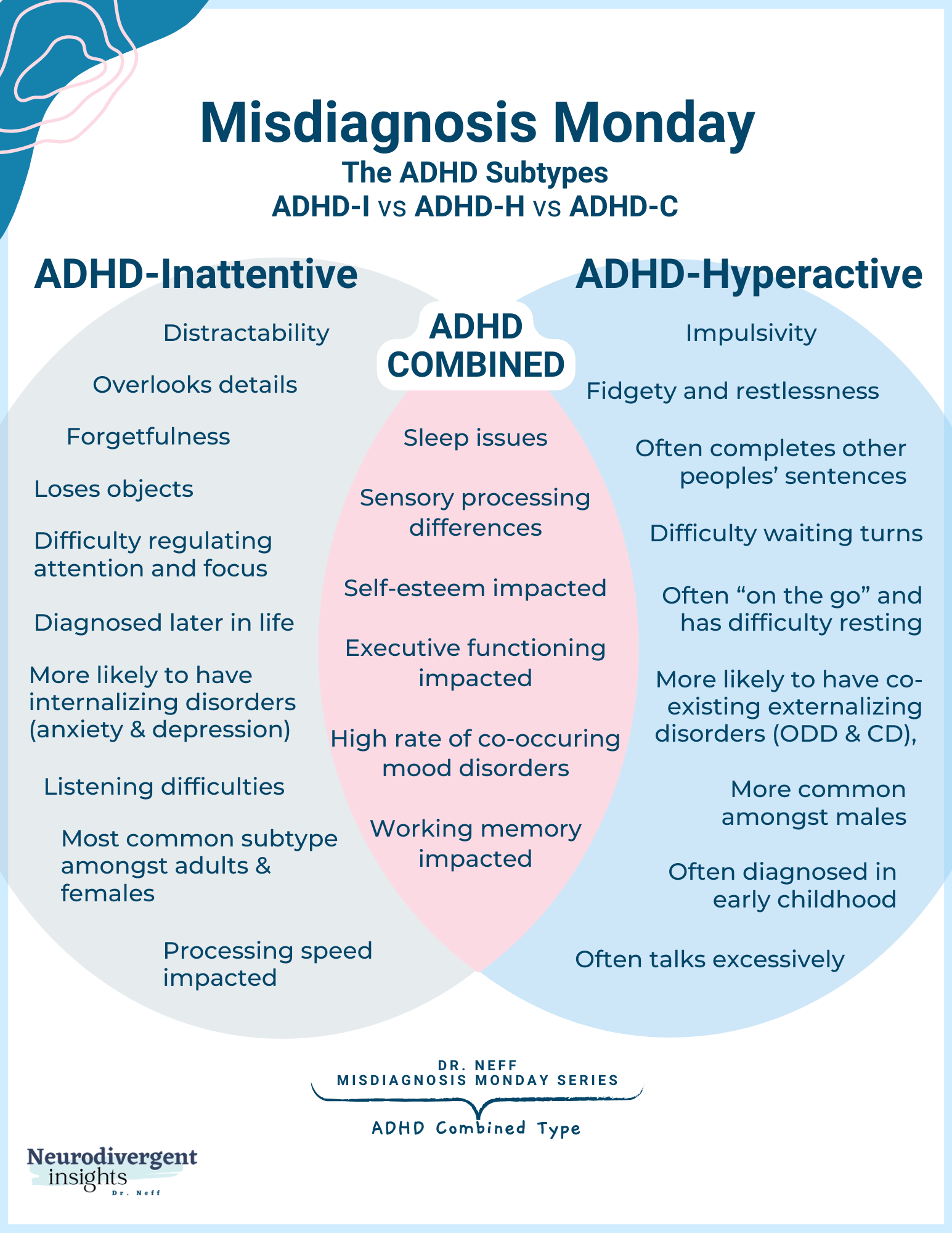
ADHD Subtypes Explained
Before leaving criteria A, let’s talk about ADHD-subtypes. There are three subtypes of ADHD that can be diagnosed. These include: ADHD-Inattentive type (ADHD-I), ADHD-Hyperactive/impulsive (ADHD-H), and ADHD-Combined type (ADHD-C).
ADHD-I is characterized by difficulties regulating attention
ADHD-H is characterized by impulsive and hyperactive behavior
ADHD-C is characterized by both inattention and hyperactivity/impulsivity
ADHD-C and ADHD-I are the most common ADHD subtypes among adolescents and adults (Bianchini et al., 2013; Willcutt, 2012).
ADHD-H is the most common subtype seen among preschoolers diagnosed with ADHD (Willcutt, 2012).
Given how the prevalence rates ebb and flow throughout the lifespan, it is helpful to think about these subtypes with a bit of fluidity. A person may meet the criteria for different subtypes throughout the lifespan. The diagnosis provided at one specific time may differ from that provided at another specific time in a person's life. For example, a young child may be diagnosed ADHD-H, and in mid-childhood, meet full criteria for ADHD-C, and in adulthood, only meet criteria for ADHD-I.
A person has ADHD or not, the ways in which the traits present at a given point in time or a given context has a great deal of flux, and thus it's helpful to hold the framework of subtypes with flexibility. Given the ebb and flow, it is likely better to think of ADHD as a whole and to consider how it may present differently throughout the lifespan.
There is a lot of debate on the legitimacy of the three subtypes of ADHD. There is increasing evidence that many people with ADHD-inattentive type experience internal restlessness (a form of hyperactivity), which may contribute to anxiety disorders and depression. Given this, I find it best not to think of these as concrete and definitive categories but rather as different phenotypes (different presentations) of ADHD.
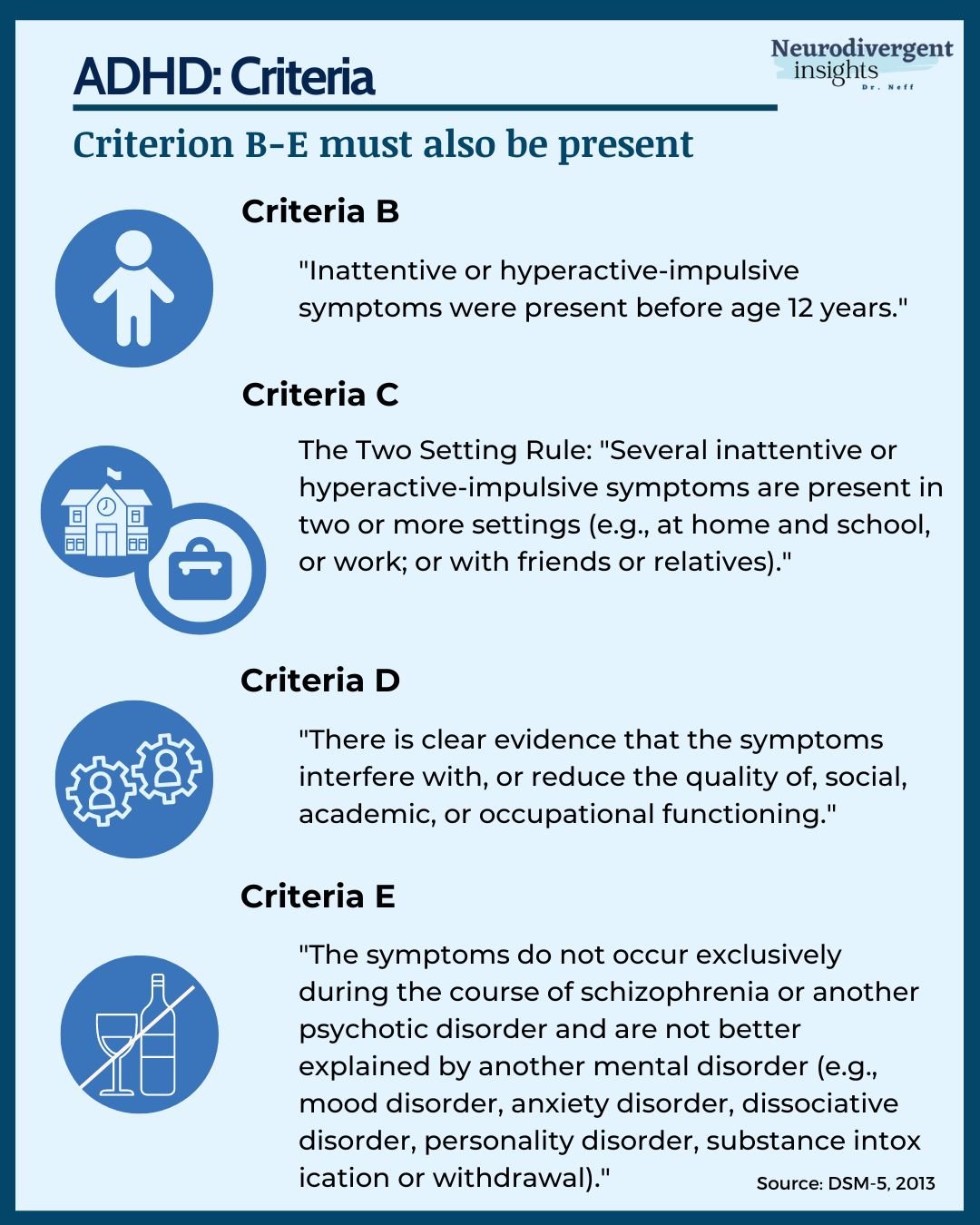
ADHD Criteria B-E
ADHD Criteria B-E
In the DSM, the last few criteria of any diagnosis code typically have to do with the disqualifies or rule-outs. The same is true here.
Criteria B: ADHD is a neurodevelopmental condition (i.e., a neurodivergence). As such, it is innate and not acquired, and there must be evidence of it from early in life. It is important to note that ADHD traits may not become apparent until the person is under undue stress or in unsupportive environments. A person may also learn to mask their ADHD traits early in life and may evade detection until adulthood.
Criteria C: As discussed above, ADHD is not situational inattention but rather a part of a person's baseline experience. One way this is commonly measured is by assessing whether or not a difficulty with inattention and/or hyperactivity is present across multiple contexts. While I appreciate that a good assessment is trying to get a sense of a person's baseline experience (vs. context or situation dependent), when this rule is rigidly applied, it can lead to misdiagnosis.
Criteria C may contribute to people with ADHD-I and ADHD-H being missed more often. Emerging research suggests that impact on functioning (i.e., impairment) has some differences among the three subtypes. While ADHD-C often shows "impairment" in both school and home (or work and home), a subset of people with ADHD-I and ADHD-H only shows significant impairment in a single setting at a single point in time (Willicutt, 2012).
ADHD-I is most likely to show impairment in school because of the attention demands. At the same time, ADHD-H is more likely to show impairment at home due to behavioral difficulties, and people with ADHD-C are the most likely to show impairment in multiple contexts. This is a significant finding as it means we are likely missing ADHD-inattentive type and ADHD-hyperactive type at higher rates.
Criteria D: To reach the threshold of a clinical diagnosis, ADHD traits must cause suffering and impair functioning. To meet any diagnosis in the DSM, this is essentially a requirement. The experiences must either "impair functioning" or cause significant distress in areas relating to school, work, or social relationships.
Criteria E essentially speaks to the importance of not conflating ADHD with other conditions that can impact attention, hyperactivity, or impulsivity. There are many conditions that can lead to difficulties with inattention, hyperactivity, and impulsivity. Criteria E is there to ensure that the clinician has ruled out other potential causes for inattention, hyperactivity, and/or impulsivity. This is particularly important when considering pharmaceutical support. If inattention and impulsivity are related to a manic episode, psychotic episode, or anxiety (versus ADHD), then putting that person on a stimulant could cause more damage. For this reason, a careful assessment is essential.
Thanks so much for following along and reading; I hope you found this helpful for better understanding the DSM-5 for ADHD. If you're interested in more conversations like these, I have many articles and e-books covering ADHD and commonly co-occurring conditions. You can learn much more over in my Misdiagnosis Monday series.
Older Images (from 2022)