Is it ADHD or ODD? How Racial Bias Impacts Diagnosis.
As a mental health therapist specializing in neurodivergent conditions, I am committed to shedding light on the systemic issues that can impact diagnosis and treatment. In a recent #MisdiagnosisMonday post, I explored the common misdiagnosis of ADHD and ODD. Today, I want to delve deeper into how the racial bias of mental health providers can contribute to misdiagnosis and further marginalize already vulnerable communities. With this post, I hope to raise awareness about the pervasive issue of racial bias in mental health care, and invite you to join me in working towards a more equitable future.
The Disproportionate Diagnosis of ODD in BIPOC Children
Did you know that ODD is disproportionately diagnosed in Black, Latino, and Hispanic children? Studies show that racial and ethnic diagnostic disparities in disruptive behavioral disorders are well-documented, particularly among urban, low-income Black American and Latino youth, (Ballentine, 2019; Coker et al., 2016). The cause of these diagnostic disparities is multifactorial, but there is growing evidence that unconscious racial bias contributes to this discrepancy in diagnosis. In fact, clinicians often over-pathologize behaviors of ethnic and racial minorities as more dangerous and disobedient, leading to diagnostic disparities (Fadus et al., 2020).
Even when controlling for confounding variables such as adverse childhood experiences, prior juvenile offenses, genetics, and socio-demographics, these diagnostic and treatment disparities remain. A white child with a similar presentation is more likely to be diagnosed with an adjustment disorder or ADHD, while racial and ethnic minorities are more likely to receive a diagnosis of a behavioral disruptive disorder like ODD (Fadus et al., 2020) These biases can lead to misdiagnosis and inadequate treatment, putting vulnerable populations at risk.
Research has shown that children from racial and ethnic minority groups are more likely to receive a diagnosis of a behavioral disruptive disorder such as Conduct Disorder (CD) and Oppositional Defiant Disorder (ODD), and less likely to receive a diagnosis of Attention Deficit Hyperactivity Disorder (ADHD) (Cameron and Guterman, 2007).
Racial Disparities in the Diagnosis of Behavioral Disruptive Disorders and ADHD
Research has shown that children from racial and ethnic minority groups are more likely to receive a diagnosis of a behavioral disruptive disorder such as Conduct Disorder (CD) and Oppositional Defiant Disorder (ODD), and less likely to receive a diagnosis of Attention Deficit Hyperactivity Disorder (ADHD) (Coker et al., 2016; Fadus et al., 2020). For instance, a study of 1173 youth living in residential treatment facilities found that Hispanic and Black American youth were diagnosed with CD at significantly higher rates than non-Hispanic white youth (43.3% and 34.4%, respectively, compared to 24.4%) (Cameron and Guterman, 2007).
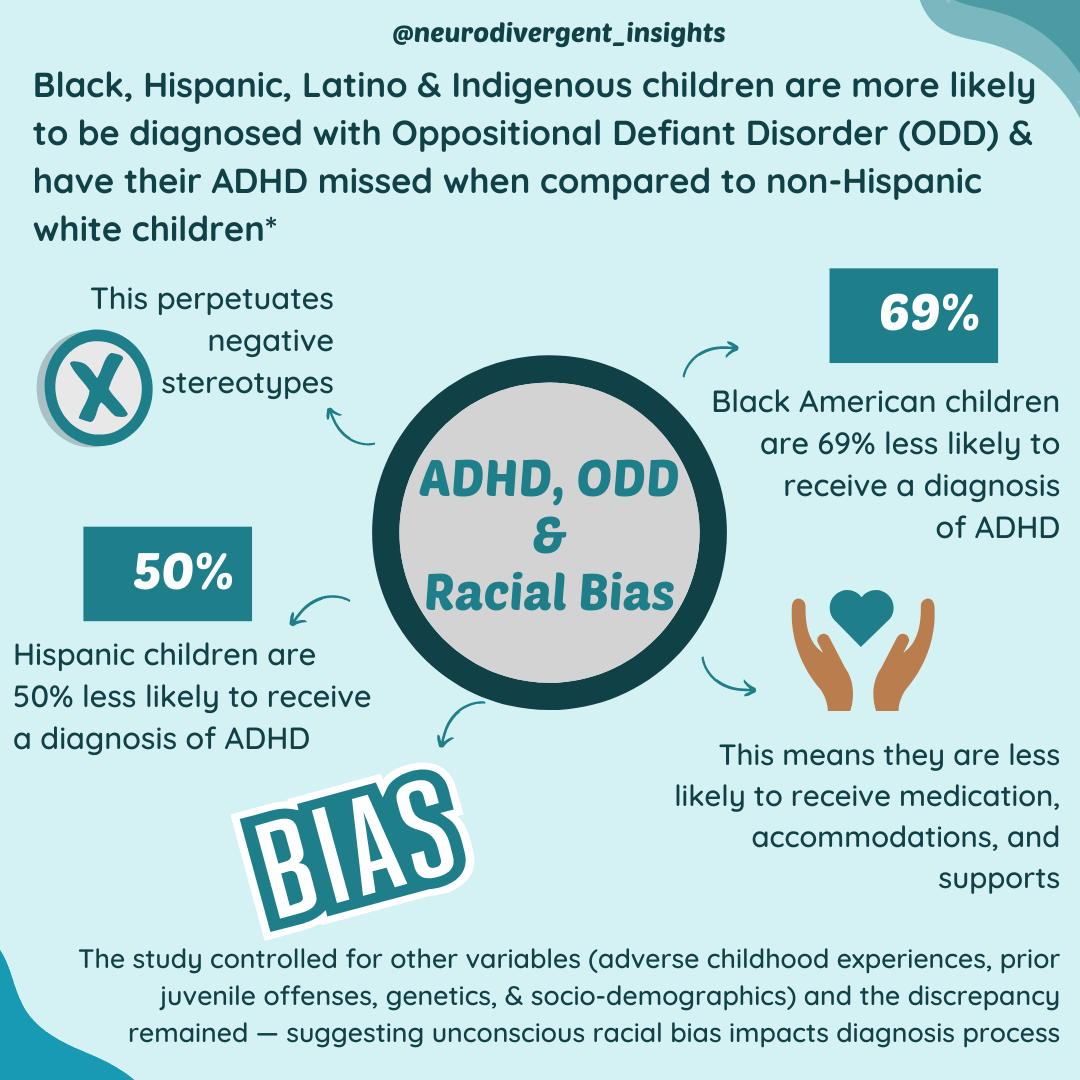
Likewise, a national representative sample of 17,100 children by Morgan et al., (2013) found that Black American children were 69% less likely, Hispanic children were 50% less likely, and children of "other races/ethnicities" were 46% less likely to receive a diagnosis of ADHD, compared to non-Hispanic white children. Even after controlling for other variables, race still significantly influenced the likelihood of receiving an ADHD diagnosis.
This discrepancy is also reflected in the national prevalence rates of ADHD. According to a national survey in 2010, the prevalence of ADHD among non-Hispanic white children was 5.6%, while the prevalence among Black American youth was 4.1%, and 2.5% among Hispanic youth (Getahun, 2013). These findings suggest that racial bias in diagnostic decision-making plays a role in the overdiagnosis of CD and ODD and the underdiagnosis of ADHD in certain racial and ethnic groups.
How Racial Bias Impacts ADHD and ODD Diagnoses: Disparities and Implications
Addressing racial bias within the diagnosis process is crucial on multiple levels. In addition to perpetuating harmful stereotypes, it can also do a disservice to a child and their family. Misdiagnosing a child with ODD and missing their ADHD diagnosis can leave them vulnerable, preventing them from accessing appropriate medications, therapies, and accommodations. As a result, BIPOC children may be at higher risk, while the disparities that exist in the medical, educational, and juvenile justice systems are perpetuated (Fadus et al., 2020).
It's important for clinicians to recognize the potential for unconscious bias to influence their diagnostic processes and be meticulous in ruling out neurodivergence before diagnosing ODD and other disruptive behavioral disorders. Studies have shown that there are significant disparities in ADHD treatment among different races, with white children being more likely to receive treatment, while Asian-Americans are the least likely to receive treatment (Shi et al., 2021). By being aware of these disparities and working to reduce the impact of racial bias, clinicians can help ensure that children receive the support and care they need to thrive.
Confronting Racial Bias in Mental Health: Moving Towards Equity and Inclusion
In summary, racial bias is a concerning factor in the diagnosis and treatment of neurodivergent children. As we've seen, children from ethnic and racial minority groups are more likely to be diagnosed with disruptive behavioral disorders such as ODD and less likely to be diagnosed with ADHD, even after controlling for other variables. These biases can have serious implications for children's access to appropriate treatments and services, leaving them vulnerable and perpetuating harmful stereotypes.
To combat racial bias and promote equity in the mental health field, it's crucial that clinicians and mental health professionals remain aware of their biases and make an effort to provide equitable care. This means acknowledging and actively working to dismantle the systemic and individual biases that exist in the medical, educational, and juvenile justice systems. It also means advocating for and prioritizing anti-racist education and training for all mental health professionals, as well as increased diversity and representation in the field.
It's time to acknowledge and address the systemic issues that lead to racial disparities in mental health diagnosis and treatment. By doing so, we can work towards a more equitable and just mental health system that truly supports all neurodivergent individuals.
Note: If you’re looking for someone who provides training at the intersection of neurodivergence and BIPOC individuals, check out the work of Living Autism Out Loud. Their organization is committed to eliminating barriers that Black, Indigenous, and People of Color (BIPOC) parents of children with Autism and other Intellectual Developmental Disabilities face when accessing services. They use family engagement training to improve service providers, educators, and community partnerships.
Citations
Ballentine KL. Understanding Racial Differences in Diagnosing ODD Versus ADHD Using Critical Race Theory. Families in Society. 2019;100(3):282-292. doi:10.1177/1044389419842765
Cameron M, Guterman N. Diagnosing conduct problems of children and adolescents in residential treatment. Child Youth Care Forum. 2007;36(1):1–10.
Coker, T. R., Elliott, M. N., Toomey, S. L., Schwebel, D. C., Cuccaro, P., Tortolero Emery, S., Davies, S. L., Visser, S. N., & Schuster, M. A. (2016). Racial and Ethnic Disparities in ADHD Diagnosis and Treatment. Pediatrics, 138(3), e20160407. https://doi.org/10.1542/peds.2016-0407
Fadus, M.C., Ginsburg, K.R., Sobowale, K. et al. Unconscious Bias and the Diagnosis of Disruptive Behavior Disorders and ADHD in African American and Hispanic Youth. Acad Psychiatry 44, 95–102 (2020). https://doi.org/10.1007/s40596-019-01127-6
Getahun D, Jacobsen SJ, Fassett MJ, et al. Recent trends in childhood attention-deficit/hyperactivity disorder. JAMA Pediatr. 2013;167(3):282–8.
Morgan PL, Staff J, Hillemeier MM, et al. Racial and ethnic disparities in ADHD diagnosis from kindergarten to eighth grade. Pediatrics. 2013;132(1):85–93.
Shi Y, Hunter Guevara LR, Dykhoff HJ, et al. Racial Disparities in Diagnosis of Attention-Deficit/Hyperactivity Disorder in a US National Birth Cohort. JAMA Netw Open. 2021;4(3):e210321. doi:10.1001/jamanetworkopen.2021.0321