PTSD and Autism
PTSD vs. AND Autism
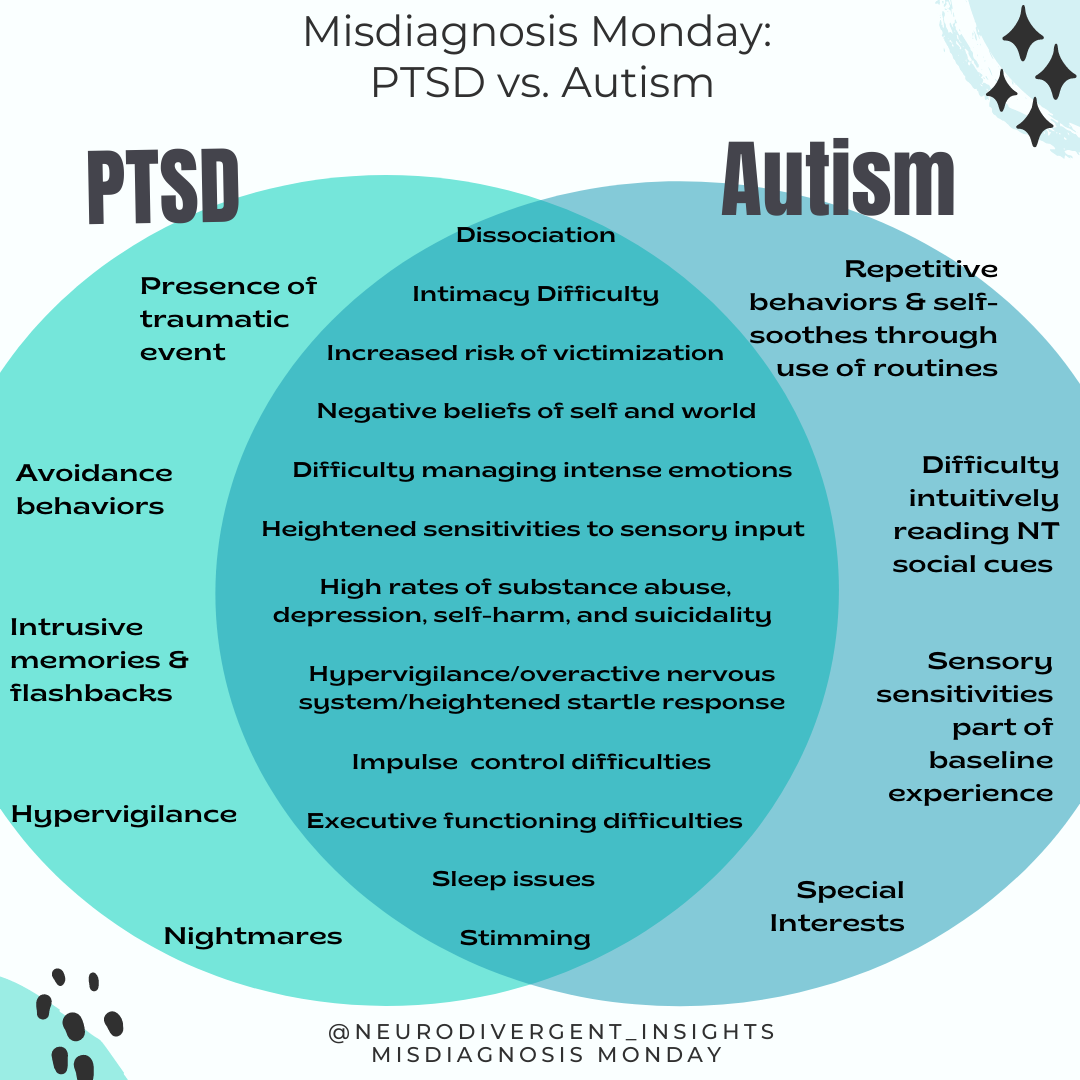
While I have set up this series to distinguish autism from common misdiagnoses, this week’s topic is more complex. You can see from the Venn Diagram there is so much overlap between PTSD and Autism! In addition to many shared experiences, they also co-occur at alarmingly high rates.
Given the high rate of co-occurrence, it is more likely that missed diagnosis happens (vs. misdiagnosis). A missed diagnosis happens when a person’s PTSD is accurately diagnosed while their underlying neurotype (autism) remains missed. When they do co-occur this creates some additional complexity in the clinical presentation. I’ll cover these topics as well as provide clinicians will some ideas on how to adapt traditional trauma treatment for the Autistic person in mind.
Contents:
Misdiagnoses
Misdiagnosis
Given the co-occurrence of Autism and PTSD, it is likely rarely a misdiagnosis (it's likely accurate), but the autism may be missed. PTSD is rarely an inaccurate diagnosis; however, when PTSD is used to explain away the Autistic traits and experiences, it may be considered a "misdiagnosis"”
Our field has much to thank for the recent development of trauma-informed care and treatment. I am thankful for the work of Dr. Burke Harris, Bessel Van der Kolk, and countless others in bringing awareness to trauma. I'm thankful for the work done to create trauma-informed spaces as more therapists, educators, and medical providers are working from a trauma-informed lens. And while I fear minimizing these crucial advancements, I believe it's important to consider the potential risk of trauma becoming the new "it" lens from which the mental health field sees everything.
I've talked with countless people whose autism was missed because their traits were explained away through the framework of PTSD or c-PTSD. In our enthusiasm to help bring healing around trauma, we (the mental health field) are vulnerable to making trauma the new "lens" from which everything is understood. The field is at risk of falling into confirmation bias as we quickly reduce all sensory and dysregulation experiences to trauma.
There are many reasons it can be hard to tease out autism from PTSD; below is a list of overlapping characteristics that can make it difficult to distinguish between the two:
Overlapping Characteristics
Sensory Sensitivities
The nervous system/amygdala goes on hyper-alert in the aftermath of trauma as a means of trying to protect against future harm. This looks similar to the sensory profile of a hypersensitive autistic.
Increased Amygdala Activation
Wiring around the amygdala, the “safety alarm,” becomes more sensitive after trauma. Research on amygdala and Autistics is mixed, but many of us have more amygdala involvement during certain activities (i.e., eye contact).
Difficulty Regulating Intense Emotions
Associated with brain chemistry (amygdala) and sensory profile, it becomes more difficult to self-soothe and regulate difficult emotions.
Increased Risk of Substance Abuse
Substances can be a powerful method of regulating a hyperactive nervous system. Both groups are at an increased risk of substance abuse disorders.
Self-Harm Behavior
Elevated within both groups. Self-harm functions to ground, self-soothe, and regulate the nervous system.
Dissociation
This is a common trauma response and can also be a response to sensory overload. Common among both groups.
Suicidality
Autistic people are 3-7 times more likely to die by suicide. Suicidality is also more common among trauma survivors.
Increased Risk of Victimization
Trauma survivors are at a higher risk of re-victimization. Similarly, recent research has demonstrated that autistic women and gender-diverse individuals are more likely to be survivors of violent victimization. Some risk factors include the challenge in social reasoning, missing contextual cues, and a tendency to take things literally. In one study, Autistic adults were 7.3 times more likely to endorse having experienced sexual assault from a peer during adolescence (Weiss and Fardella).
Given the significant overlap, it’s easy to see how one may miss the autism in favor of a PTSD diagnosis, especially if a trauma history is present. And most neurodivergent people do experience trauma, whether it is the big T trauma of victimization or the small t trauma of marginalization, bullying, and discrimination. This brings us to point 2, the intersection of Trauma and Autism:
Understanding the Intersection: Trauma and Autism
Autistics are much more likely to experience PTSD than the general population, especially women, genderqueer people, and BIPOC Autistics. Research shows Autistic women have a double vulnerability—more vulnerable to victimization and more vulnerable to developing PTSD following a traumatic event. Autistic women are 1.5 times more likely to be victimized than their allistic peers. In addition to being more vulnerable to victimization, we are also more vulnerable to developing PTSD following a traumatic experience.
There are various theories about why this is: more active amygdala, inflexible nervous systems, more difficulty regulating emotions, and our tendency to take in the sensory experience with more intensity. In fact, Rumball et al. (2020) found that we develop PTSD at higher rates even when criteria A is not met (for non-clinicians, that essentially means less intense trauma).
Here are a few sobering facts about the intersection of autism and trauma:
💙 Rumball et al. (2020) study found that approximately 60% of autistics reported probably PTSD in their lifetime (compare this to 4.5% of the general population) (Rumball, 2020).
💙 Haruvi-Lamdan et al., 2020 study found that 32% of their Autistic participants had probable PTSD compared to 4% of the non-autistic population
💙 Fenning et al., 2019 research demonstrated that autistic children had more reactive nervous systems. This aligns with similar research that has identified the autistic nervous system to be less flexible (Thapa and Alvares, 2019). Less flexible nervous systems have a more difficult time coping with acute stressors and may contribute to increased hyperactivation of the nervous system following trauma.
💙 Neurodivergent (ADHD/Autism) neurobiology is more vulnerable and reactive: (Beauchaine et al., 2013)
💙 We are more vulnerable to social victimization and marginalization. In Haruvi-Lamdan et al., 2020 females with autism (but not males) reported more negative life events, particularly social events, than typical adults.
💙 Our sensory profiles mean many of us absorb sensory experiences with more intensity. The memories and sensations thus code in our minds and bodies with more intensity.
This double vulnerability is rarely talked about as a part of Autistic Awareness or within the clinical literature on trauma. The lack of awareness around this is unfortunate as any good trauma treatment must consider the neurotype that is undergirding the experience of trauma. Unfortunately, few clinicians are trained in how to do Autistic affirming trauma work. It’s to that topic we now turn….
Autistic Trauma Treatment
As the above statistics show, autism/PTSD co-occurs at unfathomable rates. When autism is missed, the trauma treatment is negatively impacted. It is critical to treat Autistic trauma with a neurodivergent adapted approach. Just like our pathway to trauma is not the neurotypical pathway, neither can our treatment be the same as neurotypical treatment.
Don’t Skip the Basics
Grounding and relaxation strategies are the foundational blocks of any good trauma treatment. It’s necessary that the person have tools and practices that help them to re-anchor when the trauma hijacks their body. Because our nervous systems are less flexible than an allistic nervous system, it is harder for us to get back to baseline once triggered. If progress feels slow, that is okay; again, it takes us more work to get back after our nervous system has been hijacked.
Consider Somatic Therapies
We need more attention to our sensory profile (grounding, bodywork, encouraging natural forms of movement, etc.). Our sensory system is likely in intense overdrive. Our bodies are already a difficult place for many of us to occupy; trauma is like throwing gasoline on top of a sensitive sensory system. Somatic experiencing and other body-based approaches to trauma should be considered. However, given the intensity of the body experience, autonomy and empowerment for the client to move at their pace must be considered.
Adapt Exposure Therapy (If Used)
Exposure therapy is often treated as the gold standard for PTSD treatment. However, this can be quite dysregulating for the Neurodivergent person if not adopted. If used, it is critical it is adapted & client-led. Sensory experiences outside of our control are dysregulating; we must control the sensory experience. Proper attention to pacing and recovery is essential. Initial treatment must focus on increasing interoception and regulation skills before working through exposure. For more thoughts on how to adapt exposure-based treatment for Autistic clients, you can check out the list of considerations.
Be Cautious of CBT
CBT is aimed at confronting unhelpful beliefs about the world and self. The clinician must realize that these “maladaptive schemas” were not just developed in the trauma but also derived from years of being marginalized by society (often on an unconscious level). Thus, it is possible that attempting to reframe some of these negative beliefs will have a rebound effect of increasing shame and confidence in beliefs. The insistence on reframing may also result in a loss of trust in the therapeutic relationship. When used CBT should be sure to consider the experience of marginalization and early formation of core negative schemas.