Schizophrenia vs. Autism
Schizophrenia vs. Autism
(plus, a brief history of Autism)
Historically speaking, Autism is a relatively new diagnosis. Schizophrenia and Autism share a long, intertwining history. For much of the 20th century, Autistic children were diagnosed under the umbrella of Schizophrenia (childhood-onset Schizophrenia or COS).
The term autism first found its way into the literature in the early 1900s when it was used to describe the tendency for schizophrenic children to create and live in a world of their own (Vortsman and Burbach, 2014). The Swiss Psychiatrist Paul Eugen Bleuler coined the term “autism” as a key feature of Schizophrenia in 1911 (Evans, 2013).
The term was used to describe the social withdrawal and detachment from reality so often observed in children with Schizophrenia (Zeldovich, 2018). The term began to take on its own meaning as researchers began to discern differences between a subset of children who presented slightly differently and had a different trajectory than other children with Schizophrenia. It wasn’t until the research of Kolvin (1971) that Autism was distinguished from Schizophrenia, and finally, in 1980 Autism was separated from Schizophrenia in the DSM-III.
Contents:
A Brief History of Autism
It’s challenging to talk about the differences between schizophrenia and Autism without exploring the history of Autism. Or maybe it’s not challenging, but my autistic brain likes understanding and situating this conversation within the larger, historical context :)
As early as 1924, Grunia Sukhareva-a Russian Child Psychiatrist began observing and writing about distinctive features of the children she worked with. Sukhareva argued that a subset of her patients came into the world with a condition resembling schizophrenia, but that was essentially different. Namely, she observed that while her schizophrenic patients tended to decline and become less engaged with the world (more internal), a subgroup of children improved throughout their lifespan and became less inward-focused and increased in their engagement with the external world. She observed that these children had rich inner lives, describing one young boy as “an introverted type, with an autistic proclivity into himself” (Zeldovich, 2018). While at first Sukhareva used the term “autistic” in the same way intended by Bleuler, over time, she adapted it as she saw more and more boys who demonstrated these “Autistic tendencies.” She began creating more crystalized observations about these “autism tendencies.”.
In 1925 she published a paper outlining the specific traits she saw within the group of boys she was working with. She was remarkable in her insight and precision, as her early observations essentially parallel the DSM-5 current diagnosis for Autism (Zeldovich, 2018). She described a “lack of facial expressiveness,” “talking in stereotypical ways,” “strong interests pursued exclusively,” and “sensitivities to specific noises or smells” Zeldovich, 2018). Ironically, it took nearly a century for the DSM to arrive at the same conclusions Sukhareva arrived at in 1925.
Sukhareva herself was skeptical of the overlap between Schizophrenia and this emerging condition she was observing; she cautioned her colleagues that the term “schizoid” might lead to confusion and misinterpretation of this syndrome (Silberman, 2015).
As early as the 1950s, she was speculating as to different brain regions of the brain impacted by these different conditions; her speculations were later confirmed with the development of brain scans (Zeldovich, 2018). Her work was legendary, unfortunately, her work didn’t reach the English-speaking world til 1996. Had her work reached the English-speaking world earlier than it did, perhaps the confusion between schizophrenia and autism would have been cleared up long before 1980 (Zeldovich, 2018).
Autism research has not always been kind to women, including Sukhareva. Despite her research coming nearly two decades before Leo Kanner and Hans Asperger first published, she is often not talked about in Autism history, and the credit for “discovering” Autism is typically given to Kanner and Asperger. Certainly, there were some linguistic and political barriers that impacted her work being reached the English-speaking world; however, there may also be more sinister reasons behind her notable absence in Autism history.
Egos get messy when it comes to scientific discovery. There is speculation that Kanner intentionally did not cite Asperger’s work so as to appear original (Silberman, 2015). Now there is speculation that Hans Asperger intentionally did not cite Sukhareva (Zeldovich, 2018) as to appear to be the founder when he published his research. Sukhareva’s work was translated to German as early as 1925s; reasonably Asperger should have had access to her work. Given her wide publications and specialization on the topic, the absence of reference to her is notable (Zeldovich, 2018).
Hans Asperger working in Germany, and Leo Kanner writing in the context of the United States, pushed the literature forward as they further clarified the Autism phenotype. Hans Asperger also saw the overlap between schizophrenia and Autism, while also working to distinguish this new syndrome from schizophrenia. Asperger saw within the children he worked with the tendency toward what Bleuler referred to as "Autistic thinking" or the tendency toward "self-centered rumination and retreat into fantasy" (Silberman, 2015, 98).
Asperger observed how children pursued their goals with intensity and with little regard for the external world. He thus coined the term "Autisischen Psychopathen" to describe the condition of the children he worked with. In addition to describing pathology, he coined the term "Autismus" which referred to a more natural element, like when a scientist discovers a new life form (Silberman, 2015, para 98).
It almost seems as if Asperger was expressing an early idea of neurodiversity. He seemed to see it as a natural biological element and observed how it showed in a myriad of expressions. His research highlighted that Autism encompassed a vast spectrum of people--from the most intellectually gifted to the severely disabled. He highlighted that many different varieties of Autism occurred naturally within the population (Silberman, 2015).
Kanner, working at John Hopkins, in the context of the United States, took a slightly different approach. Where Asperger highlighted the wide range of the spectrum, Kanner was quicker to zoom in and rigidly define Autism as a monolithic group. Kanner primarily worked with younger children, heavily impacted by Autistic traits. Kanner’s narrative of Autism was that it was an incredible, rare and extreme condition (Silberman, 2015). Kanner primarily worked with infants and young children.
He suggested that a subset of children diagnosed with schizophrenia had an innate inability to form relationships with people, which was a separate, and rare condition that he termed early infantile Autism (Siberman, 2015). While Kanner’s work helped distinguish Autism from Schizophrenia, unfortunately, it later served to perpetuate a narrative that Autism is a rare, extreme, and monolithic condition. This was a stark difference from Asperger’s research which emphasized the broad spectrum of Autism.
Following Kanner’s work, there was speculation that infantile Autism could be an early manifestation of childhood schizophrenia (Vortsman and Burbach, 2014). During the 1960s and 1970s, this was often talked about as “early-onset psychosis” (infancy) vs. late-onset psychosis” (adolescence).
It was the work of Israel Kolvin in the early 1970s that eventually helped to distinguish the different traits of “early-onset psychosis” (characterized by Ritualistic and compulsive phenomena i.e., Autism) from late-onset psychosis (characterized by more thought disorder and hallucination symptoms i.e. schizophrenia). His work was foundational for providing a basis from which to differentiate these two conditions. Finally, in 1980, Autism was given its own categorization with the DSM-III and thus the intertangling of Schizophrenia and Autism was put to rest (Dvir, and Frazier, 2011).
Schizophrenia Overview
Like Autism, Schizophrenia is considered a spectrum condition. The schizophrenia spectrum includes schizophrenia, schizotypal personality disorder, schizophrenia-spectrum personality disorders, schizophreniform, and schizoaffective disorder. Some of the features of schizophrenia include difficulty discerning reality vs. non-reality and the presence of disorganized thought patterns, emotions, and behaviors. Schizophrenia has an element of complexity that has led to misconceptions in the media and in the culture at large.
Schizophrenia is not the same thing as having multiple personalities, and people with schizophrenia are not dangerous or violent. Many may experience hallucinations and paranoia while maintaining good insight into these experiences. Symptoms of schizophrenia can ebb and flow. So, a person may have a season of acute delusions, and hallucinations and may have seasons of “remission” where their symptoms are well-managed.
During an active episode of schizophrenia, a person struggles to distinguish between what is real vs. unreal. They may have active delusions, hallucinations, paranoid thinking, disorganized speech and thought patterns, disorganized body movement, and lack of motivation.
Use of alcohol, marijuana, stress, and loss of sleep tend to exacerbate and make symptoms worse. Additionally, underlying executive functioning difficulties may be exacerbated during a flare of symptoms (Psychiatry.org). Generally, symptoms fall into three major categories: Positive, Negative, and Disorganized (Psychiatry.org):
Positive Symptoms
(the presence of abnormal symptoms). Positive symptoms include: delusional and paranoid thought processes, auditory or visual hallucinations, perception distortions, paranoid beliefs, and thought processes.
Negative Symptoms
Negative symptoms refer to a decrease or absence of typical experiences/actions. Examples include: flat affect, difficulty with expressing emotions, diminished sense of emotions, reduced pleasure, failure to initiate activity, and sudden decrease in motivation. Other negative symptoms may involve difficulty organizing and initiating plans or limited ability to speak.
Disorganized Symptoms
Difficulty with logical and linear thinking, disordered thinking processes, bizarre behavior, and abnormal body movements. The person may have disorganized speech meaning they do not say complete sentences, and others often have difficulty understanding what they are saying.
Co-Occurrence of Schizophrenia
and Autism
After sharing nearly, a century of shared history, a great deal of effort was put forward to distinguish autism from schizophrenia. However, emerging genetic research is causing people to revisit the conversation about the potential relationship between schizophrenia and autism. Recent research suggests that there are both clinical and biological links between autism and schizophrenia, with a growing awareness of the number of genes/chromosomal variances being shared by schizophrenia and autism (Rapoport et al., 2009).
Several genes have been identified that potentially play a role in autism and schizophrenia. Interestingly several of these genes (approximately 15-25%) increase the risk of both autism and schizophrenia (Vortsman and Burbach, 2014). This discovery of this genetic overlap has led to new conversations about the shared phenotypes and shared etiological and biological pathways for both conditions (Vortsman and Burbach, 2014). Furthermore, these conditions appear to co-occur at higher rates than in the general population.
One study of Autistic adults found that 7.8% had co-occurring schizophrenia. Stahlberg et al., 2004
Elevated rates of autism among people with childhood-onset schizophrenia have been observed.
Two large studies found that COS (childhood-onset schizophrenia) was preceded by a co-morbid autism/pervasive development disability (PDD) in 30-50% of cases (Rapoport et al., 2009).
In the coming years, we will likely do new research that helps us understand the phenotypic and biological overlap and co-occurrence of these conditions with more precision.
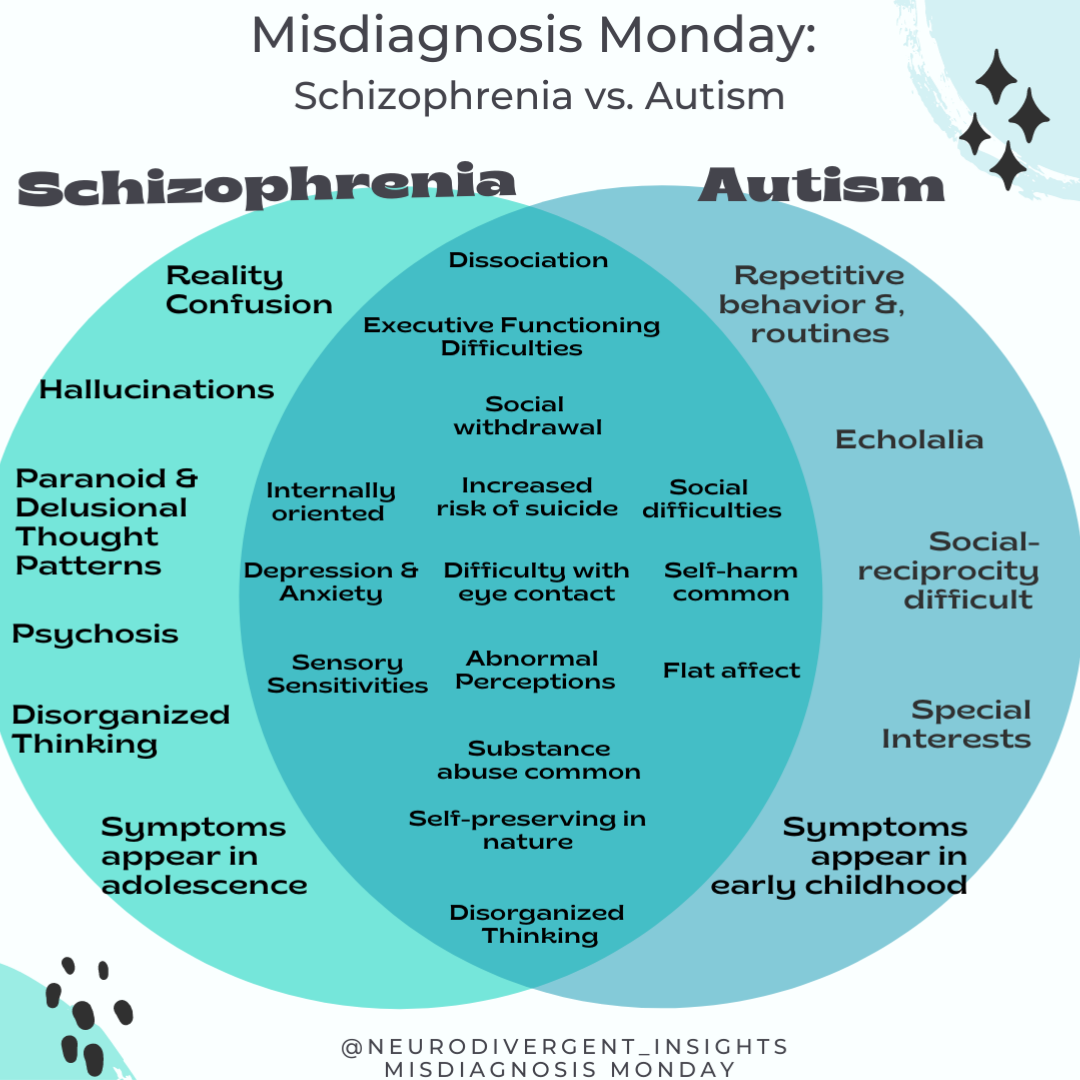
Overlapping Traits
Abnormal Perceptions/Paranoid Thinking
Hallucinations, abnormal perceptions, and paranoid thinking are core features of schizophrenia. Interestingly, Autistics are three times more likely than the general population to have hallucination-like experiences (Milne, 2017; Milne et al., 2017). Psychosis/hallucinations, like Autism, is also on a spectrum. They can be intense and can lead to a blurring of reality/non-reality, or they can be fainter in nature (the knock you thought you heard, the music you hear playing in the background, the touch you thought you just experienced).
Autistic adults experience more abnormal perceptions (hearing, sight, sound, touch). It is believed neurotransmitters, and social isolation/discrimination, may all be involved. The following information comes from the research of Elizabeth Milne.
Abnormal perceptions are distinct and different from sensory sensitivities.
47% of autistic adults answered yes to the question: “Do you ever see shapes, lights, or colors even though there is nothing there?” (compared to 14% of the control).
63 percent of Autistic adults answered yes to the question: “Do you ever feel that someone is touching you, but when you look, nobody is there?” (compared to 7 percent of the control) (Milne, 2017)
Other abnormal perceptions include strange body sensations such as experiencing a burning sensation and strange feelings in the body, hearing one’s own thoughts or fearing those near you can hear your thoughts.
Autistics were more likely to report experiencing distress associated with their abnormal perceptions.
Speculated that abnormal perceptions may be related to altered GABA levels in the autistic bran
Past research has shown that those who experience isolation and discrimination (such as in the case of migration) also have more hallucinatory and paranoid feelings than people who are not discriminated against. Bullying, discrimination, and social isolation related to Autism may thus increase the risks of hallucinatory and paranoid feelings.
In the context of autism, the auditory perceptions/hallucination-like experiences are on the milder end of the psychic spectrum. Having an experience that causes one to be unable to distinguish reality from non0reality (i.e., psychosis) could not be attributed to autism alone.
Sensory Differences
Hyper and hypo-sensory sensitivities are well-known features of Autism. And this is a lesser-known feature of Schizophrenia. Recent research suggests that there can also be sensory dysfunctions in the context of Schizophrenia: Javitt, 2009). Differences in the auditory system (hearing) are the most widely documented area of sensory concern among people with schizophrenia.
Executive Functioning Difficulties
Both Autistics and people with Schizophrenia tend to experience executive functioning difficulties, including difficulty with cognitive flexibility, task-switching, memory, and attention. For the person with Schizophrenia, their executive functioning tasks tend to get worse during an acute onset of systems (Orellana and Slachevsky, 2013).
Early Symptom Overlap
Children with both may present with language delay, social withdrawal, be prone to fantasy, and a tendency to get “lost” in their internal world.
Paranoid and thought disorganization
Disorganized thinking and paranoia are well-known features of Schizophrenia. Many autistic people experience significant anxiety when under pressure which can present as disorganized thinking or paranoid thinking. This tends to worsen when they are asked to task-switch amidst pressure/anxiety (Berney, 2000). Autistics who have experienced discrimination and bullying are also more vulnerable to paranoid feelings and thought patterns.
Social-Relational Traits
Social withdrawal, communication impairment, and poor eye contact seen in ASD are similar to the negative symptoms seen in people with Schizophrenia (Posey et al., 2004).
Neuroimaging Studies (Gray Matter)
In a study done by Cheung et al., 2010. people with ASD and Schizophrenia had lower gray matter volumes within limbic-striato-thalamic neurocircuitry. There were slight variations, as the gray matter was reduced in the amygdala, caudate, and frontal and medial gyrus for Schizophrenia, while it was reduced in the putamen for Autism. Cheung et al. demonstrated clear overlap in terms of brain volumetrics, suggesting that Autism and Schizophrenia likely share a common etiology.
Psycho-Social Risks
In addition to overlapping phenotypes. We also share many psycho-social risks.
Self-Harm: In one study, 50% of patients with schizophrenia reported a history of Self-Harm. This was increased among females, those with depression, and those experiencing suicidality (Mork et al., 2012). Similarly, self-harm is high among autistics with average to high IQs. One study found that parents reported self-harm behavior among autistic youth in 15% of cases (Huang).
Suicidality: Both groups have an increased risk of suicidality and an increased risk of dying by suicide. Approximately 4.9% of people with schizophrenia die by suicide (Palmer et al., 2005); rates are higher among men and among those who have co-occurring substance conditions (Hor et al., 2010) Autistics with average to high IQ are three times more likely to attempt or die by suicide than the general population (South et al.). Suicidality was particularly high among youth and young adults and was more elevated among women than men (South et al.)
Substance Abuse: Substance abuse is high among both groups. Nearly half of people with schizophrenia will have a substance abuse disorder at one point in their life Volkow N. D. (2009). A recent study in Sweden found that folks with Autism with average to high IQs were twice as likely to struggle with addiction to alcohol or other drugs.
Victimization: Autistic adults are at an increased risk of experiencing interpersonal violence. In one study, Autistic adults were 7.3 times more likely to endorse having experienced sexual assault from a peer during adolescence (Weiss and Fardella). Fitzgerald et al. 2005 study found an increased risk of victimization (both violent and non-violent victimization) among people with schizophrenia. And women with schizophrenia have higher rates of being sexually victimized (Goodman and Harris, 1995).
How to Spot the Difference
Criteria A of autism may look like Negative symptoms of Schizophrenia. And so, it is critical to assess for Criteria B symptoms of Autism and Positive symptoms of Schizophrenia to get a complete clinical picture.
Focus on Criteria B for Autism
Given criteria A symptoms may overlap with Schizophrenia negative symptoms, it is essential to assess for the presence of criteria B symptoms (rigidity and repetitive behaviors, special interests, sensory issues). If a clinician is assessing for Schizophrenia but not considering ASC, they won’t assess for these things, and ASC may be missed. The RAADS can be a helpful tool for assessing some of the criteria B traits.
1. Repetitive, stereotyped movements, use of objects, and/or speech (i.e., stimming, repeated vocal phrases, lining up or categorizing objects).
2. Inflexibility of behavior and thought, ritualistic behaviors, concrete thinking (i.e., echolalia, listening to songs on repeat, adherents to routine, tendency to take things literally, and being high context thinkers)
3. Intense interests and/or attachment to objects (i.e., Special interests)
4. Sensory processing symptoms (under-reactivity, over-reactivity, or fascination with sensory input.
Assess for Positive Symptoms of Schizophrenia
When assessing for Autism, if you aren’t also considering Schizophrenia, you may discount negative symptoms of Schizophrenia as criteria A for Autism. If it doesn’t occur to you to rule out schizophrenia, you may not consider assessing for positive symptoms of schizophrenia, and thus Schizophrenia may be missed. To assess positive symptoms, include consideration of delusional thought patterns, paranoid thoughts, and the presence of hallucinations. However, be aware that abnormal perceptions are more common among autistic adults. Overall patterns, the intensity of paranoia and hallucinatory experiences, and the level of insight into the experiences must be considered (i.e., is there good insight into reality vs. non-reality).
Consider using Routine Screeners
The AQ and RAADS are standard routine screeners for Autism (you can find a roundup of several free screeners here. For Schizophrenia, consider using the EPS9 or EPS26. While there is an online version, consider that clients with active paranoia may prefer the paper version.
EPS9 (online version): https://apps.telesage.com/sage/clinic/free/eps9
Paper version: https://secureservercdn.net/198.71.233.15/5fb.b8d.myftpupload.com/wp-content/uploads/2021/06/EPS-9-print.pdf?time=1624897841
EPS26 (Paper version) https://secureservercdn.net/198.71.233.33/5fb.b8d.myftpupload.com/wp-content/uploads/2020/03/EPS26-TeleSage.pdf
Citations
Cheung C, Yu K, Fung G, et al. Autistic disorders and schizophrenia: related or remote? An anatomical likelihood estimation. PLoS One. 2010;5:e12233.
Berney TP. Autism-an evolving concept. Br J Psychiatry. 2000;176:20-25.
Evans B. (2013). How autism became autism: The radical transformation of a central concept of child development in Britain. History of the human sciences, 26(3), 3–31. https://doi.org/10.1177/0952695113484320
Fitzgerald, P. B., de Castella, A. R., Filia, K. M., Filia, S. L., Benitez, J., & Kulkarni, J. (2005). Victimization of patients with schizophrenia and related disorders. The Australian and New Zealand journal of psychiatry, 39(3), 169–174. https://doi.org/10.1080/j.1440-1614.2005.01539.x
Harrison, K. B., McCredie, M. N., Reddy, M. K., Krishnan, A., Engstrom, A., Posey, Y. S., Morey, L. C., & Loveland, K. A. (2020). Assessing Autism Spectrum Disorder in Intellectually Able Adults with the Personality Assessment Inventory: Normative Data and a Novel Supplemental Indicator. Journal of autism and developmental disorders, 50(11), 3935–3943. https://doi.org/10.1007/s10803-020-04450-2
Javitt D. C. (2009). Sensory processing in schizophrenia: neither simple nor intact. Schizophrenia bulletin, 35(6), 1059–1064. https://doi.org/10.1093/schbul/sbp110
Hor, K., & Taylor, M. (2010). Suicide and schizophrenia: a systematic review of rates and risk factors. Journal of psychopharmacology (Oxford, England), 24(4 Suppl), 81–90. https://doi.org/10.1177/1359786810385490
Kolvin. I. 1971. Infantile Autism, Concepts Characteristics and Treatment in Infantile Autism, Concepts Characteristics and Treatment, M. Rutter (ed.) "Psychoses in childhood - a comparative study", pp. 7-26. (Link to chapter)
Kolvin, I. (1971) Studies in childhood psychoses: I. Diagnostic criteria and classification. British Journal of Psychiatry, 118, 381–384.CrossRef
Milne E, Dickinson A, Smith R (2017) Adults with autism spectrum conditions experience increased levels of anomalous perception. PLoS ONE 12(5): e0177804. https://doi.org/10.1371/journal.pone.0177804
Mork, E., Mehlum, L., Barrett, E. A., Agartz, I., Harkavy-Friedman, J. M., Lorentzen, S., Melle, I., Andreassen, O. A., & Walby, F. A. (2012). Self-harm in patients with schizophrenia spectrum disorders. Archives of suicide research: official journal of the International Academy for Suicide Research, 16(2), 111–123. https://doi.org/10.1080/13811118.2012.667328
Orellana, G., & Slachevsky, A. (2013). Executive functioning in schizophrenia. Frontiers in psychiatry, 4, 35. https://doi.org/10.3389/fpsyt.2013.00035
Palmer BA, Pankratz VS, Bostwick JM (2005). The lifetime risk of suicide in schizophrenia: a reexamination. Arch Gen Psychiatry, 62(3):247-53. [PubMed] [Ref list]
Posey DJ, Kem DL, Swiezy NB, et al. A pilot study of D-cycloserine in subjects with autistic disorder. Am J Psychiatry. 2004;161:2115-2117.
Stahlberg O, Soderstrom H, Rastam M, Gillberg C. Bipolar disorder, schizophrenia, and other psychotic disorders in adults with childhood onset AD/HD and/or autism spectrum disorders. J Neural Transm. 2004; 111:891-902.
Rapoport, J., Chavez, A., Greenstein, D., Addington, A., & Gogtay, N. (2009). Autism spectrum disorders and childhood-onset schizophrenia: clinical and biological contributions to a relation revisited. Journal of the American Academy of Child and Adolescent Psychiatry, 48(1), 10–18. https://doi.org/10.1097/CHI.0b013e31818b1c63
Silberman, S. (2015). Neurotribes: The legacy of autism and the future of neurodiversity. Penguin.
Volkow N. D. (2009). Substance use disorders in schizophrenia--clinical implications of comorbidity. Schizophrenia bulletin, 35(3), 469–472. https://doi.org/10.1093/schbul/sbp016
Vorstman J.A.S., Burbach J.P.H. (2014) Autism and Schizophrenia: Genetic and Phenotypic Relationships. In: Patel V., Preedy V., Martin C. (eds) Comprehensive Guide to Autism. Springer, New York, NY. https://doi.org/10.1007/978-1-4614-4788-7_96
Zeldovich, L. 2018. How history forgot the woman who defined autism. Autism Spectrum Research. Retrieved October 16, 2021: https://www.spectrumnews.org/features/deep-dive/history-forgot-woman-defined-autism/